So Comfortable You Can’t Even Feel It! The Cocaine Tampon
By Gemma Angel, on 29 April 2013
 by Lisa Plotkin
by Lisa Plotkin
Last May, a Utah woman was in for a surprise when she purchased a $1.99 box of tampons from a local store in Salt Lake City. Instead of a cotton tampon inside the applicator, the woman discovered something else with a much steeper price tag: cocaine. At first she was completely astonished and didn’t realize it was cocaine – she thought that the cotton might have somehow disintegrated; so unlikely was the pairing of cocaine and tampons to her. Similarly, when the police were called in to collect the cocaine, they too expressed their surprise at this method of transporting drugs. Detective Carlie Wiechman, spokesperson for the Salt Lake City Police Department, said this in response to the crime: “It’s not every day we run across this. We run across different ways of packaging and distributing, but it never ceases to amaze us the different and creative ways of trying to move drugs around.”
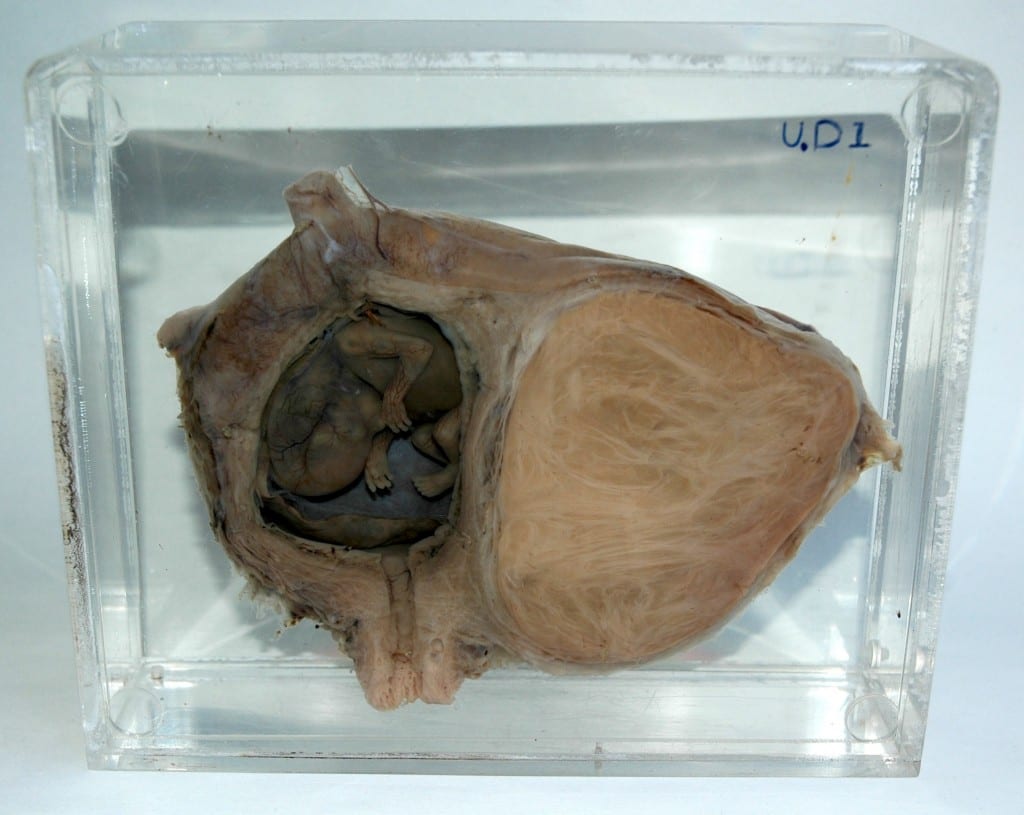
However, the marriage of cocaine and tampons is not as farfetched or creative as the Salt Lake City PD imagined, and for 19th century surgeons and gynecologists it was a regular – dare I say it, ‘everyday’ – medical sight. Throughout the 19th and early 20th centuries, cocaine was regularly used as a local anesthetic in surgery. It was often administered in the form of what doctors referred to as a tampon – a medical device invented in the 18th century primarily as an antiseptic to clog up bullet wounds. The tampon was traditionally soaked in whatever antiseptic or anesthetic drug was in general use, before being applied to a wound. These tampons were not particularly associated with women; at least not until later in the 19th century that is, when cocaine came to be regarded as an especially effective treatment for gynecological diseases.
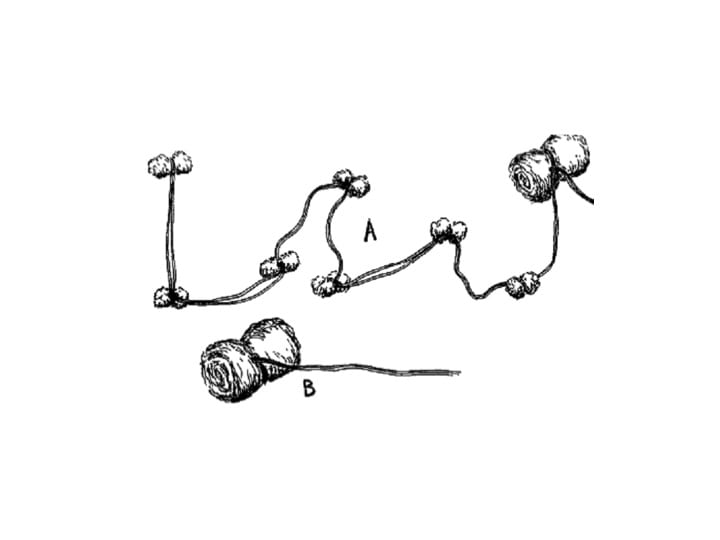
A: Kite-tail tampon; small wads of cotton tied together
on one string with a fairly large tampon on the end.
B: Ordinary rolled tampon.
Image from Practical Clinical Gynecology in:
American Journal of Surgery, vol. 39, issue 1 (1938).
Cocaine was believed effective against a whole range of women’s ailments: From painful intercourse; to uterine diseases; to cervical endometritis; to inflammation of the urethra; to dysmenorrhea – the list goes on and on. [1] In fact, cocaine was even believed to assure a ‘painless childbirth’ and according to Physician to the British Lying-in Hospital, John Philipps, could even cure the scourge of ‘sore nipples’. [2].
How would the cocaine be applied in these situations? A typical gynecological answer: by vaginally “inserting a tampon soaked in a freshly prepared solution of 2 % cocaine through a narrow Ferguson’s speculum.” [3]
Therefore, with regards to many women’s diseases, the question was not should cocaine be used- but how much. This was common until the interwar period. Of course, accidents do happen and sometimes these tampons were never removed, (most were). To read more about other ‘accidental’ foreign bodies left behind in women’s bodies, read my previous blog post here. Although many women were on board with the idea of being treated with cocaine, some did however refuse. So, the Utah woman who recently discovered cocaine in her tampon carton was by no means the first to say ‘thanks, but no thanks’ to tampons with coke on the side!
Learn more about our current UCL exhibition on all kinds of foreign bodies see.
References:
[1] Stephen R. Kandall: Women and Addiction in the United States (Cambridge, MA: Harvard University Press, 1996).
[2] John Philipps: ‘The Value of Cocaine in Obstetrics’, in The Lancet (26 November 1887), p. 1061
[3] ‘A Note on the Morphine-Hyoscine Method of Painless Childbirth’, in British Medical Journal (6 January 1917).
 Close
Close