The Smartphone Dilemma: Exploring Parental Decision-Making for 9-12 Year Olds
By CBC Digi-Hub Blog, on 10 May 2023
Written by Rachel Perowne, PhD Student (UCL Centre for Behaviour Change)
Children’s interaction with the online world is a hot topic – recently, The Economist magazine asked whether smartphones are to blame for recent increases in the rates of suicide among girls [1]. This week, the Children’s Commissioner for England published a report evidencing the effect of pornography on harmful sexual behaviour among children and suggesting a link between exposure to pornography and children being given their own phones at younger ages [2].
I was 21 when I got my first mobile phone and over 30 when I got my first smartphone, but today’s children and young people are growing up in the digital world where the concept of a ‘brick phone’ or landline is alien, and smartphones are the norm. As technology plays an ever-increasing role in our lives, it’s not surprising to learn that children are acquiring smartphones at a younger and younger age. To illustrate, in 2018, 35% of 8–11-year-olds owned a smartphone [3] and this had risen to 60% by 2022 [4].
So how do parents make the decision to give their child a smartphone?
This question fascinated me – both as a parent with a son approaching 11 years old and as a researcher interested in young people’s wellbeing in a digital world. I could hear many of my friends and peers with children of a similar age debating what to do and I took the opportunity, whilst waiting for my PhD to officially begin, to examine this, with the support of my supervisor Prof Leslie Gutman.
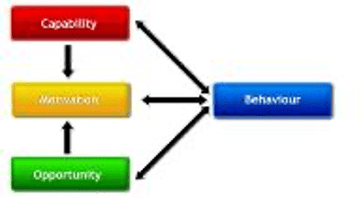
Our study, published this month, on parents’ perspectives of their children’s smartphone ownership [5], involved interviewing 11 mothers and fathers of 9- to 12-year-old children and using the COM-B model to identify which elements of Capability, Opportunity and Motivation were influencing their decision making.
Our analysis identified a number of influencing factors across all three COM-B domains:
- The external environment was a key enabling factor in parents deciding to give their child a smartphone; parents see smartphones as an inevitable aspect of the modern world that can only be resisted for so long because ‘technology is everywhere’.
- Added to this, the pressure of peers being given a smart phones – the social opportunity – creates a ‘domino effect’ which then affects parents’ motivation, making them want to prevent their children being left out and help them build their social relationships.
- They also see advantages in being able to track their child’s movements and ensure they are contactable once they start travelling independently to and from school. ‘When they… go to school by themselves, then obviously I need to give the smartphone’. Hence the transition from primary school is a key time for many children being given a smartphone.
- However, parents are conflicted. They also have worries about their children entering the world of smartphones and the unfettered access to the internet that this can bring. ‘Having his phone in his room at night is a big worry for me’.
- They worry about the impact of social media, about bullying, about overuse and addiction but are sometimes unsure of what the real benefits and risks are. ‘I think there are certain risks and I think there are certain benefits but it’s all kind of in my own head’.
This uncertainty is understandable. Evidence is mixed on the impact of smartphones on younger children, with many recognising that smartphones can support learning and increase digital skills which are important for life in a technological world. At the same time, whilst causal linkages are hard to demonstrate, correlations are apparent between smartphones and sleep disturbance, anxiety and academic performance. It seems clear that young people are also particularly prone to Problematic Smartphone Usage (where usage interferes with daily life and activities).
So where to go from here?
The parents we spoke to were grappling with their decision-making. They felt that there was a lack of guidance and support for them in planning how and when to give their child a smartphone. This challenge is heightened because their own digital technology skills and knowledge are often inferior to their child’s, meaning that their efforts to control usage and access can be undermined by a tech-savvy child. Our paper discussed potential intervention strategies (using the Behaviour Change Technique Taxonomy (v1) [6] including:
- Restrictions such as having a recommended minimum age for smartphone ownership
- Guidance and support for parents preparing and planning to give a child their first smartphone
- Education from credible sources on the benefits and risks of smartphones for children
- Training in setting up appropriate controls on a child’s smartphone
Whether there is a role for regulation and restriction (such as age limits) of smartphones is a debate that rages. In either case, it seems clear that expecting parents to navigate this significant decision on their own is too much. Given the potentially lasting impacts of owning a smartphone for children, better guidance and support from authoritative, trusted sources are required.
[5] Perowne, R., & Gutman, L. M. (2023). Parents’ perspectives on smartphone acquisition amongst 9-to 12-year-old children in the UK–a behaviour change approach. Journal of Family Studies, 1-19. https://www.tandfonline.com/doi/full/10.1080/13229400.2023.2207563https://www.tandfonline.com/doi/full/10.1080/13229400.2023.2207563
[6] Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M., Cane, J, & Wood, C. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behaviour change interventions. Annals of Behavioral Medicine, 46(1), 81–95.
Designing for engagement with digital behaviour change interventions: state of the art and chartering new territories
By CBC Digi-Hub Blog, on 14 February 2022
Written by Dr Kristina Curtis (UCL Centre for Behaviour Change)
This blog article is dedicated to a panel discussion from the CBC Conference Enabling Behaviour Change to Build Back Better for health & sustainability: 1 – 3 Nov 2021. An interdisciplinary panel of experts took us on a journey from how we define and measure engagement to how we learn from big data and produce a generalisable science of factors that promote engagement.
We kicked off the engagement panel with Dr Kevin Doherty from Technical University Denmark, who began his quest to conceptualise engagement from a review of the computer science literature. Kevin was struck by the wide range of perspectives and conceptualisations of engagement from ‘a quality of user experiences with technology’ (O’Brien and Toms, 2008) to ‘..the phenomena of being captivated and motivated’ (James et al. 2011). To help understand where these different perspectives were coming from, Kevin and his team turned to the original theories, revealing a huge range from most cited Flow Theory (50 mentions) to least cited Richness Theory (2 mentions). Still struggling to pin down what exactly was meant by engagement, Kevin and his team looked next at measurement for further insights. They uncovered a long list of measures such as questionnaires, behaviour logging, facial analysis, and gesture tracking. Next, they looked at the design strategies used to design for engagement and reported a variety of strategies including recommendations such as ‘usability’, ‘immersing users’ and ‘inspiring fun’. As these strategies were employed across a range of contexts and technologies, they were still no closer to pinning down exactly what was meant by ‘engagement’. A combination of Kevin’s applied work and academic review led to thinking about engagement not only in terms of what it is, but how we might design for engagement as a process and how users engage with technology as a process in itself. Kevin ended his talk around remaining challenges, one being how we build interdisciplinary teams and the necessary knowledge to facilitate this kind of approach to engagement.
Our next panellist was Professor Rik Crutzen from Maastricht University brought us on to the topic of measuring engagement. Rik stated as with any psychological construct, it’s important to ‘disentangle’ this conceptualisation from how it is measured. These are not two separate entities but related to one another. As with measuring psychological constructs, we use a plethora of methods to measure engagement such as surveys and reaction times. Interestingly and in contrary to some of the audience’s views, Rik argued against a standardised way of measuring engagement. Instead we ought to keep a ‘decentralised’ meaning, as ultimately it will depend on the context and how we are conceptualising engagement in the first place. Rik’s second point related to the distinction between measuring intended and actual use of an intervention and methods employed to understand usage behaviours. For example, ‘Think aloud’ procedures can help to uncover if certain user groups go to different places on a website and whether any content is misinterpreted, allowing an organisation to continually refine their intervention. Rik’s final point addressed the novel ways to reduce participant burden and increase engagement. For example, avatars can be used as a proxy for psychological constructs and skip logic in questionnaires can help to reduce participant burden via shorter questionnaires. Indeed, reducing participant burden is key to sustaining users’ engagement with an intervention and must be prioritised.
Next on the stage was the panel’s industry expert: Charlotte Summers COO and Director of Research at DDM Health. Charlotte Introduced GRO – a digital platform providing disease-specific education, behaviour change support and feedback to optimize health and wellbeing. Gro has been developed with leading clinicians to address all modifiable risks. Charlotte shared encouraging research findings from peer-reviewed published health outcomes including: Type 2 diabetes remission, weight loss, reduce medication, reduced anxiety, depression and perceived stress. So, what’s in this successful platform? Charlotte described the following features: personalised resources; one-to-one behaviour change coaching; goal setting; community support and integrated tracking. It also uses AI software to optimise engagement and health outcomes. This platform is a patient-healthcare platform to allow real-time health monitoring and engagement information. Charlotte demonstrated through a case study how ‘big data’ can be used to provide answers on intended vs actual use. They noticed that it was actually the younger family members using the app on behalf of their older relatives that did not speak the language or were not digitally literate. These insights allowed them to further refine the app and offer even more personalisation, with a recognition that is important to engage not just the individual, but the family as a whole in helping to manage type 2 diabetes.
The final panellist was Dr Olga Perski from UCL who took us through a stimulating presentation on whether current approaches are getting us closer to identifying ‘timeless’ design elements. Olga drew our attention to the current state-of-the-art around identifying design elements that reliably influence engagement. This of course is important for designing websites/apps that people want to use and saves money through reduced testing of design iterations. Olga’s talk highlighted the importance of an interdisciplinary team with expertise in how we use a combination of user-centred design (e.g., co-design workshops) and experimental methods (e.g., factorial trials) to better understand design elements that influence engagement with health and wellbeing websites/apps. Findings from these kind of research methods have provided important insights on broader design elements such as ‘ease of use’, ‘personalisation’, and ‘interactivity’ which are important drivers of engagement. However, the challenge exists in the myriad of ways these design elements can be operationalised. One could argue, this is also where the creativity and innovation comes into play and again the importance of testing design features with the relevant target audience. In addition, Olga points out that design preferences will change over time and across contexts, which is in part due to the changing social and cultural norms/expectations. Research shows that users tend to rely heavily on “social proof” to help navigate which technologies to adopt. With deeply contextual and ever changing social, cultural norms and expectations, it’s looking increasingly challenging to identify “timeless” design elements…For example, although chatbots were seen as moderately acceptable by internet users in 2019, they will likely be more commonplace and widely acceptable in 2030. So, what’s the solution? Olga left us with the idea of embracing complexity. In line with the common theme running throughout this discussion panel, design principles, as with the conceptualisation and measurement of engagement, will largely depend upon context.
Papers panellists drew on are listed below:
Doherty, K et al (2018). A mobile app for the self-report of psychological well-being during pregnancy (BrightSelf): qualitative design study. JMIR mental health, 5(4)
Doherty, K., & Doherty, G. (2018). Engagement in HCI: conception, theory and measurement. ACM Computing Surveys (CSUR), 51(5), 1-39
Doherty, K., & Doherty, G. (2018). Engagement in HCI: conception, theory and measurement. ACM Computing Surveys (CSUR), 51(5), 1-39
Doherty, K. (2019). Designing the Self-Report of Wellbeing in Pregnancy (Doctoral dissertation, Trinity College Dublin).
Doherty, K et al (2018). A mobile app for the self-report of psychological well-being during pregnancy (BrightSelf): qualitative design study. JMIR mental health, 5(4)
Metz, G., Roosjen, H., Zweers, W., & Crutzen, R. (in press). Evaluating use of web-based interventions: an example of a Dutch sexual health intervention. Health Promotion International.
Perski, O., Blandford, A., West, R., & Michie, S. (2017). Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Translational behavioral medicine, 7(2), 254-267.https://doi.org/10.31234/osf.io/zhj86
Perski, O., & Short, C. E. (2021). Acceptability of digital health interventions: embracing the complexity. Translational Behavioral Medicine.
Saslow, L. R., Summers, C., Aikens, J. E., & Unwin, D. J. (2018). Outcomes of a digitally delivered low-carbohydrate type 2 diabetes self-management program: 1-year results of a single-arm longitudinal study. JMIR diabetes, 3(3), e12
Short, C.E., DeSmet, A., … & Crutzen, R. (2018). Measuring engagement in e- & mHealth behaviour change interventions: viewpoint of methodologies. Journal of Medical Internet Research, 20, e292. https://doi.org/10.2196/jmir.9397
Short, C.E., Smit, E.S., & Crutzen, R. (in press). Measuring psychological constructs in computer-tailored interventions: novel possibilities to reduce participant burden and increase engagement. The European Health Psychologist. https://doi.org/10.31234/osf.io/hz593
Integrating Behaviour Change Theories with the Adaptive Decision-Making Framework
By CBC Digi-Hub Blog, on 25 May 2021
Written by Dr Chao Zhang (Department of Psychology, Utrecht University)
For someone new to behaviour change research, the large number of behaviour change theories is both a blessing and a curse. Yes, you have many options in terms of selecting a theory as the basis of your intervention, but you may also get lost in the ocean of theories. When I started my PhD project, I certainly struggled to decide which theory to use as the backbone of my thesis. This was partly because of my working environment. In the Human-Technology Interaction group at a technical university, my supervisors generally had a very pragmatic approach and were not committed to any particular theory, so I had all the freedom to explore. It was also due to my personality and intellectual style. I am not a person who easily commits myself to a particular idea, but prefer to have an overview on things and to connect pieces of ideas together. So the adaptive decision-making framework started as a literature review of behaviour change theories in my first year as a PhD student. With the encouragements from fellow PhDs and senior researchers, who found my review to be really useful, it is now a published paper in the Journal of Medical Internet Research.
Why a new framework for behaviour change theory integration?
While I was researching the literature, my urge to connect theories was accompanied by a growing discontent with many popular theories in the field. I was influenced by several articles criticising traditional behaviour change theories, but no one inspired me more than the 2011 article by William Riley and colleagues. They almost bluntly asked the question in their title: “…are our theories up to the task [of informing digital interventions]?.
One criticism they raised was the mismatch between the temporal granularities of behaviour representations used in traditional theories and digital interventions. Many of the popular theories used today were invented in the 70s or 80s, when there were no technologies available for observing or altering behaviours as they happen in people’s daily lives. For example, the famous “stage model” describes behaviour change as going through 5 stages that usually last for weeks or months, so interventions based on this theory are tailored to these coarse stages. In contrast, an e-health app on your phone can adapt its intervention strategy in almost real-time, as long as there is a need for an adaptation, e.g., to match the momentary context of a user or to tailor intervention messages to the user’s personal progress on a specific day. To inform the design of such apps, we need theoretical frameworks that match to the temporal granularity of lifestyle behaviours and digital technologies.
Another problem with traditional theories is that many of them are variable theories that describe statistical relationships between variables rather than process theories that explain the underlying mechanisms or cognitive processes of behaviour change. Variable theories are often represented visually by nodes of behaviour and behavioural determinants and the links between them that denote statistical or causal relationships. For example, based on the links connecting attitude, intention and behaviour in the Theory of Planned Behaviour, if you know the attitude of a person towards physical exercise at a certain time, you can most likely predict their exercise behaviours in the following period with some level of certainty. However, besides its predictive value, the theory does not tell you much about how to change attitude or intention in order to change behaviour, or what the cognitive processes behind the statistical relationships are. Since I was trained partly in applied cognitive psychology, I was aware of many other psychological theories that focus on processes and mechanisms, such as habit formation, reinforcement learning and decision-making. Models from these areas have certainly been applied to behaviour change interventions, but they are still not at the central stage of the field. Therefore, I was motivated to integrate such process theories into a new framework.
What is the “adaptive decision-making” framework?
When I say “behaviour change” in this blog, I almost exclusively refer to lifestyle behaviour change, not just any behaviour change. This distinction is crucial for understanding the “adaptive decision-making” framework in our paper. Some interventions may target single-time health decisions, such as a decision to receive a vaccination or not. These decisions are very consequential and usually require a lot of thinking from the decision-makers. But changing the behaviour requires nudging people to choose differently only once. However, lifestyle behaviours are about routines, habits and how people behave repeatedly, e.g. on a daily or hourly basis. For example, eating one meal of high-fat food won’t do any harm, but continuously following a high-fat diet increases one’s risk of obesity. Accordingly, lifestyle interventions should target the repeated meal choices in a person’s diet, not just a single meal choice. The characteristics of lifestyle behaviours naturally determined how behaviour change processes are represented in our framework. Instead of “stages” or a diagram of interlinked variables, behaviour change is represented as a series of repeated and interrelated decisions (see Figure 1).
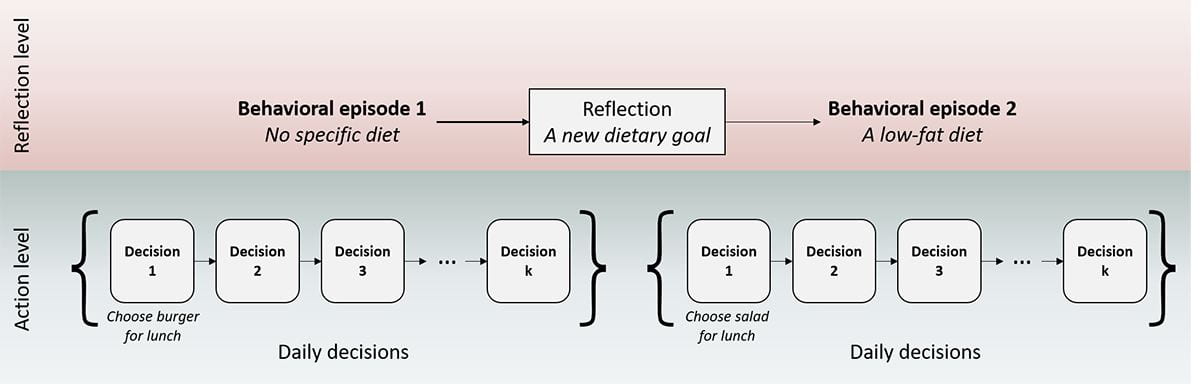
Figure 1. A two-level representation of lifestyle behaviour (change). Reproduced with permission from Zhang et al. (2021).
To give an example of what repeated decision-making means, let’s suppose you just started a new job and you eat your lunch everyday at the canteen of your organisation. Each day, you are exposed to different lunch options and you make your choice based on several considerations, including taste, nutritional aspects, and price. Over time, you explore different foods at the canteen by trying them out, and eventually you end up with alternating between a few of your favourite options based on your personal goals at the time. Your lunch behaviour remains habitual for a while, until you change your personal goal(s). For instance, you may become aware of your health risks after a medical test, and after some deliberation you decide to follow a low-fat diet. You take this goal into consideration when making your lunch choices and gradually you may change your lunch habit.
By considering daily decisions as the building blocks of behaviour change, the temporal granularity of the theoretical framework is matched to that of digital interventions. Even if a person tends to behave in a certain way for a certain time period, the framework allows individual decisions to vary, and at each time a decision is made, it may be affected by a different intervention (or no intervention). This representation of how lifestyle behaviours unfold over time also makes it clear what are the different explananda in a behaviour change process. First, we need to explain how individual daily decisions are made and what factors influence them. These decisions do not occur in isolation, so we also need to explain how a decision and its associated outcomes influence a person’s subsequent decisions. Finally, the adaptive decision-making framework distinguishes reflection-level processes from action-level processes. In addition to the individual daily decisions, occasionally there are also reflective moments when people set up new goals or reconsider their goals based on self-monitoring of daily behaviours. We also need to know how these reflection-level processes work. The two-level representation allowed me to integrate a wide range of theoretical ideas in psychology into a single framework, including decision-making, self-control, reinforcement learning, habit, implementation intentions, and goal-setting (see Figure 2). You can read more about how the framework was developed and its component parts in the published article.

Figure 2. A full representation of the adaptive decision-making framework. Reproduced with permission from Zhang et al. (2021).
How can the framework be used?
When I was struggling with revising the paper, my supervisor encouraged me by saying that many researchers would thank me for the paper because I did an important and difficult job for them. Indeed, I think the framework can help many researchers, especially those who just step into behaviour change research, to navigate through the literature more efficiently. Before discussing the framework, our paper also includes a review of important individual theories of behaviour change. There are of course other excellent introductory materials that give a more comprehensive overview, such as the ABC of Behaviour Change Theories, but our paper can be read as a supplement to facilitate a deeper understanding of the connections among the individual theories and one’s own ideas for theory integration.
Several other practical uses of the framework are discussed in the paper, including, for example, the identification of intervention techniques based on cognitive constructs and processes in the framework or combining multiple intervention techniques. Here I want to emphasise one specific use, i.e., the development of computational models of behaviour change based on the framework. For my own PhD work, the framework is the starting point for building computational models for the specific processes in the framework. Many people have argued for the advantages of computational models over verbal theories in behaviour change research (e.g., see this article by Spruijt-Metz and colleagues). A particular practical advantage is that computational models are essentially computer programs, which means they can be readily implemented in digital intervention systems for adaptive interventions. This is the core idea behind the psychological computing approach to digital lifestyle interventions proposed in my PhD thesis. For interested readers, this preprint describes our recent work on modelling habit formation and use of the model for better behaviour prediction in behaviour change trials. I would be very grateful if our framework inspires more research in this direction.
Notes
- I use “I” as the pronoun most of the time in this blog post because I want to tell my personal story behind the paper. However, the paper would not be possible without the contribution and support of my co-authors and amazing supervisors – dr. Daniel Lakens and prof. dr. Wijnand A. IJsselsteijn.
- I also want to express my appreciation for the PRIME theory by Robert West and colleagues. The PRIME theory is the closest to our work among all theoretical frameworks in the literature. Even though I worked out most of the framework before discovering the PRIME theory, I was certainly assured after reading it that I was going in the right direction.
Biography
Chao Zhang is currently a post-doc researcher in the Department of Psychology at Utrecht University and he is a coordinator of the HUMAN-AI alliance program. He obtained his PhD from the Human-Technology Interaction Group at Eindhoven University of Technology. He has broad interests in topics such as habit formation, behaviour change, cognitive modelling and human-centered artificial intelligence. He is keen on applying theory-based computational models to digital behaviour change interventions.
Email: chao.zhang87@gmail.com
Webpage: https://www.uu.nl/medewerkers/CZhang3
Twitter: @forzazhang
Environmental sustainability in digital health
By CBC Digi-Hub Blog, on 2 April 2021
This blog features an interview with Dr Guillaume Chevance, following his talk about environmental sustainability in digital health delivered as part of a newly formed discussion group on ethical considerations in digital health research, led by UCL researchers Dr Olga Perski, Dr Melissa Oldham and Dr Claire Garnett. You can watch Guillaume’s talk here. If you are a researcher interested in joining the discussion group, please e-mail olga.perski@ucl.ac.uk.
Can you tell me a bit about your research background?
I have a Master’s degree in Sport Sciences, with a focus on rehabilitation and physical activity. After having developed and implemented physical activity interventions for people living with chronic health conditions, I became interested in behavioural science. I therefore did another Master’s degree in Human Movement Sciences with a major in Health Psychology. I then did a PhD at the intersection of Health Psychology and Rehabilitation; the topic of my thesis was to understand the role of specific motivational factors in the regulation of physical activity in adults living with chronic conditions and participating in rehabilitation programs. Following my PhD, I did a post-doc focused on eHealth at the University of California, San Diego.
How did you come become interested in digital health and environmental sustainability?
Thanks to my mother, ecology has always been a frequently discussed topic at home. Similar to most human activities, I knew (or had the feeling, to be more precise) that too much digitalisation in the healthcare sector would not be sustainable. An interview with a French engineer, Philippe Bihouix, further sparked my interest in this topic and after reading a couple of his books, I learnt more about the issue of digital health and environmental sustainability. In 2019, a think tank called the Shift Project wrote a report called “Lean ICT: toward digital sobriety” and their conclusion was pretty straightforward:
“…the current trend of digital consumption in the world is unsustainable in terms of the supply of energy and materials that is required…”
Approximately at the same time, a colleague and good friend of mine, Paquito Bernard from the Université du Quebec à Montréal, wrote a piece for the health psychology community titled “Health Psychology at the age of the Anthropocene”. All these texts combined motivated me to try to disseminate the results from the Shift Project’s report to the eHealth community, summarised in a commentary titled “Digital health at the age of the Anthropocene”.
What’s the Anthropocene?
The Anthropocene is an unofficial geologic epoch, coined by biologist Eugene Stormer and chemist Paul Crutzen in 2000. It is used to describe the most recent period in the Earth’s history when human activity started to have a significant impact on the planet’s climate and ecosystems. Crutzen suggested that the start date of the Anthropocene should be placed near the end of the 18th century, about the same time as the start of the industrial revolution. The Anthropocene is also related to the concept of “The Great Acceleration”, which refers to the increasing human pressures on the Earth’s ecosystems (notably post-World War II) (see Figure 1). To me, the Anthropocene is a kind of a last call to avoid generalised forms of environmental and societal collapses in the next decades.
 Figure 1. Illustration of “The Great Acceleration” across different sectors and domains. Reproduced from Steffen et al. 2015.
Figure 1. Illustration of “The Great Acceleration” across different sectors and domains. Reproduced from Steffen et al. 2015.
What are, in your opinion, the most important digital health related threats to the environment?
Technically, and according to the Shift Project and other experts, the two main threats are related to (i) the rapidly growing energy consumption of the information and communication technology sector and (ii) issues of soil pollution and resources scarcity related to the rare metals that are required to build the infrastructures supporting this sector. Specifically, it seems that the explosion of video streaming and consumption of digital devices with short life spans are the main drivers of these threats. The growing electricity consumption is incompatible with the Paris Agreement and the soil pollution issue is related to both the extraction of the metals required for information and communication technologies and the lack of recycling when those digital products reach their end of life. Instead, digital devices are usually exported to low- and middle-income countries as e-waste.
Beyond environmental threats, there is also proven cases of child labour in the mines where the metals required for our digital infrastructures are extracted. Further, most rare metals are produced in conflict zones or areas controlled by monopolistic entities, which causes environmental problems and creates fragility in supply chains. These issues, coupled with inherent planetary resource limits, raise questions about our capacity to continue to access and build health devices in the future.
In my opinion, and more philosophically speaking, we who live in high-income countries are stuck in a “growth mentality”. We are always looking for more and accelerating everything. Instead, I believe it’s time to slow down so as not to further accelerate climate change and mitigate against some of its already observable implications and to leave space to communities in low- and middle- income countries to develop their digital infrastructures and reduce inequalities in this domain.
What suggestions do you have for how to overcome these environmental challenges?
The key thing for me is that we have to slow down our digital consumption. I believe that the healthcare sector, because of its laudable goals, might deserve prioritisation over other sectors (e.g., entertainment; advertising), but the size of the problem is so important that, even for health, environmental consequences should be accounted for when scaling up e- and mHealth technologies. Low-tech options requiring fewer environmental resources (e.g., simpler telemedicine solutions, well-designed text message programmes or phone-based interventions) should be prioritised over high-tech solutions promising a new digital health era made up of artificial intelligence and big data and we need to get better at recycling digital devices (see, for example, this brilliant initiative called RecycleHealth). I am not arguing against scientific and technological progress, but rather that high-tech solutions should be kept for very specific problems of high societal relevance and not scaled-up to everything and for everyone, as is often argued these days. You can read more about suggested mitigation strategies in our commentary.
Biography
Dr Guillaume Chevance is Associate Research Professor and Head of the eHealth Group at the Barcelona Institute for Global Health (ISGlobal).
Using behavioural science to increase engagement with online learning: Reflecting on a term of online delivery
By CBC Digi-Hub Blog, on 15 December 2020
Written by Dr. Danielle D’Lima, Senior Teaching Fellow for the MSc in Behaviour Change at University College London.
Due to the global pandemic, I have spent a lot of time thinking about converting the face-to-face versions of our core modules to online versions. To accommodate learners from across the globe and make best use of online pedagogy, I took the approach of dividing the content into a mixture of asynchronous and synchronous online learning activities.
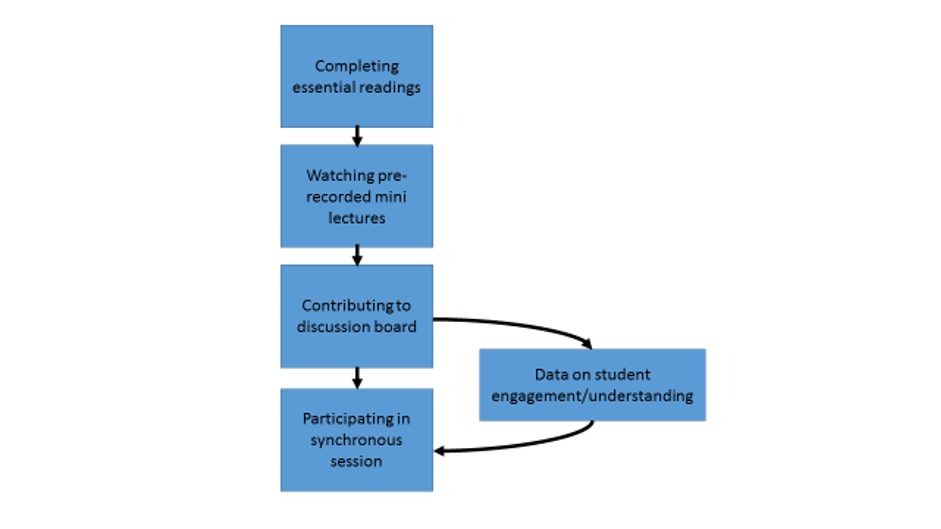
Asynchronous activities consist of essential readings, watching short pre-recorded mini-lectures and contributing to online discussion boards. These can be completed in students’ own time and pace, and are followed by a two-hour synchronous seminar in which students are supported to complete small group tasks in break-out rooms and receive some additional content developed by us based on the ‘data’ accumulated from their discussion board contributions.
This blog post offers some reflections from my experience of a term of online delivery of behaviour change teaching and considers how behavioural science itself can support us in further increasing student engagement with online learning in the future.
Over the summer of 2020, I worked on translating the teaching materials for online delivery, including chunking the lecture content to create a series of pre-recorded mini-lectures. To chunk the lecture content, I began by reviewing all of the lectures that I usually give on each module and separating the content into ‘meaningful’ sections. A meaningful section equates to a chunk of learning that stands alone but is clearly connected to what comes before and after it.
I went through several iterations of chunking in this way and recording, as I found that recording a section sometimes made me think about chunking it in a different way, and this had implications for the overall organisation of the material. The final pre-recorded mini-lectures ranged in length according to the content and purpose. For example, some took three minutes to introduce a task for the discussion board or prepare students for the upcoming synchronous session, right up to twenty minutes to cover key content for the week’s learning objectives. I was excited to undertake this exercise as I was drawn to the idea of categorising the content and reassessing it against the learning objectives. I then continued to make small iterations week by week to ensure that I could adapt and develop the mini-lecture chunks based on my experience of teaching the new MSc cohort, and the feedback I received from students across the term. For example, for Week 2, I added a short mini-lecture chunk which contained some reflections on Week 1 and additional examples to support further learning.
How has it gone so far?
The experience of Term 1 (October-December 2020) has been really positive. I have gained so much as an educator that I would not have got from delivering the content face-to-face. Despite regularly reflecting on the individual lectures that I give and how to improve them, it is sometimes difficult to see the relationships between smaller chunks of information (and the learning activities that they are nested in) after having delivered the entire content.
This approach has also helped me to address some of the specific teaching challenges that come from having a very mixed student audience from different disciplinary backgrounds. Our course covers multiple theories and models of behaviour change. Some students have relatively advanced experience and understanding of certain theories and models (e.g. those that have come to the MSc directly from a psychology undergraduate degree). However, we also have many students (around half) on our course who come from other disciplinary backgrounds (e.g. economics, arts, law, politics, history, business, and health) and therefore come to the module with no or very little prior knowledge of these theories and models.
Through the process of chunking the lecture content, I organically began to identify components that were of particular relevance to different subgroups of students (i.e. those with more or less prior knowledge or experience). I was therefore able to highlight this in my audio by clearly signposting who it was most relevant to. I could also tailor the learning where appropriate by creating and highlighting particular recordings that go into more detail on some of the theories and models. This has hopefully helped students to better understand the position that they are sitting in within the cohort, and how they can ensure that they take what they need from the pre-recorded mini-lecture chunks; it gives them autonomy to engage with the material in a way that best suits their learning needs.
I have noted that this tailored approach also has a positive impact on the synchronous sessions that I am running. For example, students are able to join the session with the right level of information to engage fully in the interactive group tasks, and I am able to join the session with prior information on how students have engaged with the asynchronous activities and the extent to which they have met the learning objectives. By having access to the ‘data’ on the discussion board in advance of each synchronous session, I have been able to proactively tailor the session in a way that I would not when delivering the lecture and seminar as part of the same face-to-face session. This offers an additional safety net to ensure that the learning objectives are successfully met for all students.
Where next?
After receiving positive and encouraging feedback from our students, I plan to take the same approach to online teaching in Term 2. However, the next module, “Behaviour Change Intervention Development and Evaluation”, will present slightly different challenges. For example, it is a highly interactive module that relies on students having the time and space to practice key skills for intervention design. I anticipate that chunking the material will help me to identify exactly which components of the material are essential for setting students up to practice and develop the skills – either independently or as part of synchronous group work – interspersed with formative feedback.
Summary of techniques used to increase engagement with online learning:
- mixture of asynchronous and synchronous activities
- chunking of lectures
- feedback
- signposting
- tailoring
- autonomy
How can behavioural science support us in further increasing student engagement with online learning?
As behavioural scientists, we have a unique advantage in understanding what students might need in order to engage with online learning. Engagement, after all, is a behaviour or set of behaviours and we know that in order to enact a behaviour people require capability, opportunity and motivation!
I include below some early reflections on what capability, opportunity and motivation might look like in the context of engagement with online learning and how we, as educators, could go about better supporting our students. These ideas are not intended to be exhaustive but instead food for thought about how we can better apply our skills as behavioural scientists when designing and delivering online education.
Capability
Students require the necessary knowledge and skills to engage with online platforms and complete the required learning activities. Clear communication to students regarding what they need to do and how they should go about doing it is essential. For example, this may involve sending a weekly alert to students explaining exactly what is expected of them in advance of the next synchronous session. Allowing students to practice interacting with the online learning environment can also go some way in supporting development of the necessary skills.
Opportunity
With numerous learning activities being allocated to students from multiple modules, there is a risk of them becoming overwhelmed. Students require sufficient time and resources to complete the learning activities (e.g. engage with the materials in advance of live sessions) and this needs to be incorporated into the planning of the activities (e.g. ensuring materials are available with sufficient time). Students also need reliable online learning platforms that are well designed and easy to navigate.
Motivation
It is important that students understand how learning activities were designed and why they are worth engaging with. By clearly communicating the rationale to students, where appropriate, educators can help them to identify the potential outcomes of their efforts. It is also important that students are rewarded for their efforts. For example, by providing informative responses to student discussion board posts and using key themes from the discussion board activity to develop teaching content.
Of course, educators themselves also need the capability, opportunity and motivation to demonstrate the behaviours required for successful online teaching (e.g. pre-recording a lecture, creating learning activities, communicating to students, etc.). But I will save that for another blog!
Bio
Dr Danielle D’Lima is the Senior Teaching Fellow for the MSc Behaviour Change at the Centre for Behaviour Change, University College London. Her role includes designing and delivering teaching and training as well as overseeing research projects on implementation science and health professional behaviour change. She also has an evolving interest in the application of behaviour change science to teaching and training.
 Close
Close