Early Career Innovators: Understanding the Role of Brain Oxygenation in Multiple Sclerosis, Devices & Diagnostics TIN
By Alina Shrourou, on 17 February 2021
In this next Devices & Diagnostics TIN interview as part of the Early Career Innovators series, acknowledging the amazing translational work being done by early career researchers within the UCL Therapeutic Innovation Networks (TINs), Dr Frédéric Lange highlights his Devices & Diagnostics TIN (co-lead by the UCL Institute of Healthcare Engineering’s Translational & Industry Delivery Group) Pilot Data Fund awarded project, “Understanding the role of brain oxygenation and metabolism in the pathophysiology and prognosis of relapses and progression in multiple sclerosis”.
Please give an overview of your research and the project that has been funded by the TIN Pilot Data Fund.
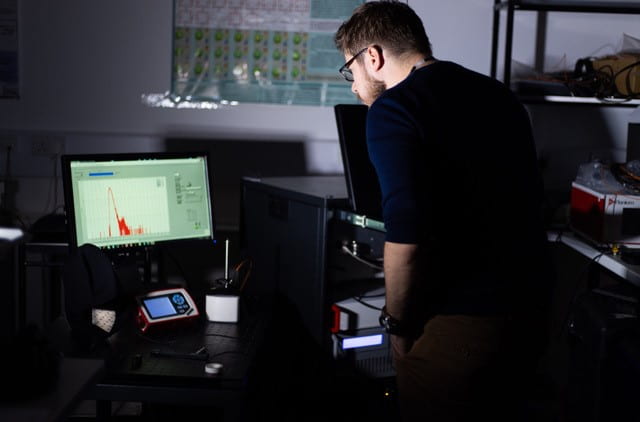
I am a biomedical engineer/physicist with a focus in biophotonics. Since I started my PhD, I’ve been working on using near infrared light to monitor the human brain physiology. Indeed, light in that range can probe deep tissues like the brain, giving us access to very useful information on tissue oxygenation or metabolism. If you are interested in that subject, I recommend consulting our public engagement website, https://metabolight.org, that explains the basics of the physics and engineering of what we do, and how we use our systems in the clinic.
The title of my TIN Pilot Data project is “Understanding the role of brain oxygenation and metabolism in the pathophysiology and prognosis of relapses and progression in multiple sclerosis”. In this project, I will use an optical instrument that I developed with some colleagues, to collect information on brain’s oxygenation and energy levels in people with multiple sclerosis (pwMS).
What is the motivation behind your project/therapeutic?
MS is the most common cause of non-traumatic disability in young adults, affecting 131,720 people in the UK. UCLH alone treats more than 5000 people with MS. Despite advances in treatments, at 17 years post-diagnosis, 11% of patients cannot walk unaided, and 18% enter a progressive form of the disease. Identifying additional mechanisms of disease progression and which patients are most likely to benefit from additional treatments therefore represents a huge unmet need.
All current MS treatments target neuroinflammation, yet substantial pre-clinical and clinical data suggests a causal role of hypoxia. We hypothesise that our instrument will allow us to identify those pwMS with the greatest such deficits, hence allowing:
- Enrichment of future clinical trials testing interventions aimed at reversing these processes.
- The monitoring the patient’s response to such treatment.
Why did you want to apply to the Devices & Diagnostics TIN Pilot Data Fund?
The Devices & Diagnostics TIN Pilot Data Fund was a great opportunity for me as it was perfectly fitting the stage of my current research. Indeed, I was just finishing the developmental phase of the instrument that I wanted to build, and I was transitioning to its use in the clinic. With my clinical colleague, we could start to use the instrument on patients, but we realized that a few changes were needed in order to facilitate its use in a clinical environment, so we needed to make some adjustments. However, it can be difficult to find funds at this stage of a project, as it is not an engineering project anymore, but at the same time, it is not a clinical project yet. We needed some preliminary data on patients in order to be able to apply to a more clinically focused grant. So, this kind of fund is perfect to close the gap between an engineering and clinical project.
Moreover, from a more personal point of view, this fund was a good opportunity to apply to my first independent grant, which I hope will be the first step towards my independent career.
Learn more about TIN opportunities for researchers
What do you hope to achieve in the 6 months duration of your project and what are the next steps from now?
With this project, I will be able to upgrade my existing optical instrument, so it is easier to use in the clinical environment and more robust. The fund will be used to buy the essential components needed to make these upgrades. I am currently purchasing the equipment needed. The upgrade process will occupy the first half of the project, between the hardware and the software work, and the recalibration of the system. Then, in the second half of the project, we will aim to scan as many pwMS as possible, so we can have a good set of preliminary data. This will certainly prove challenging in these trouble times, but I am confident that we will be acquire some very useful data.
About Dr Frédéric Lange
Dr Frédéric Lange received his Ph.D. degree in biomedical optics from the University of Lyon and INSA de LYON in France in 2016. Since then, he has been a Research Associate with the Biomedical Optics Research Laboratory, which is part of the Department of Medical Physics and Biomedical Engineering at UCL.
His main research interests are in the development of diffuse optics instrumentation and methodologies for biomedical applications, especially for brain monitoring.
 Close
Close