In this Repurposing TIN interview as part of the Early Career Innovators series, acknowledging the amazing translational work being done by postdoc and non-tenured researchers within the UCL Therapeutic Innovation Networks (TINs), Dr Pilar Acedo highlights her Repurposing TIN Pilot Data Fund awarded project, involving the repurposing of gene P53 reactivators to treat pancreatic cancer.
What is the title of your project and what does it involve?
My project is entitled ‘Repurposing p53 reactivators for the treatment of pancreatic cancer’. TP53 is frequently mutated in pancreatic ductal adenocarcinoma (PDAC), the most prevalent type of pancreatic neoplasms, and these mutations are associated with poor outcomes, making mutant p53 (mtp53) an attractive target. Having higher levels of reactive oxygen species (ROS) compared to normal cells, cancer cells are more sensitive to further oxidative insult.
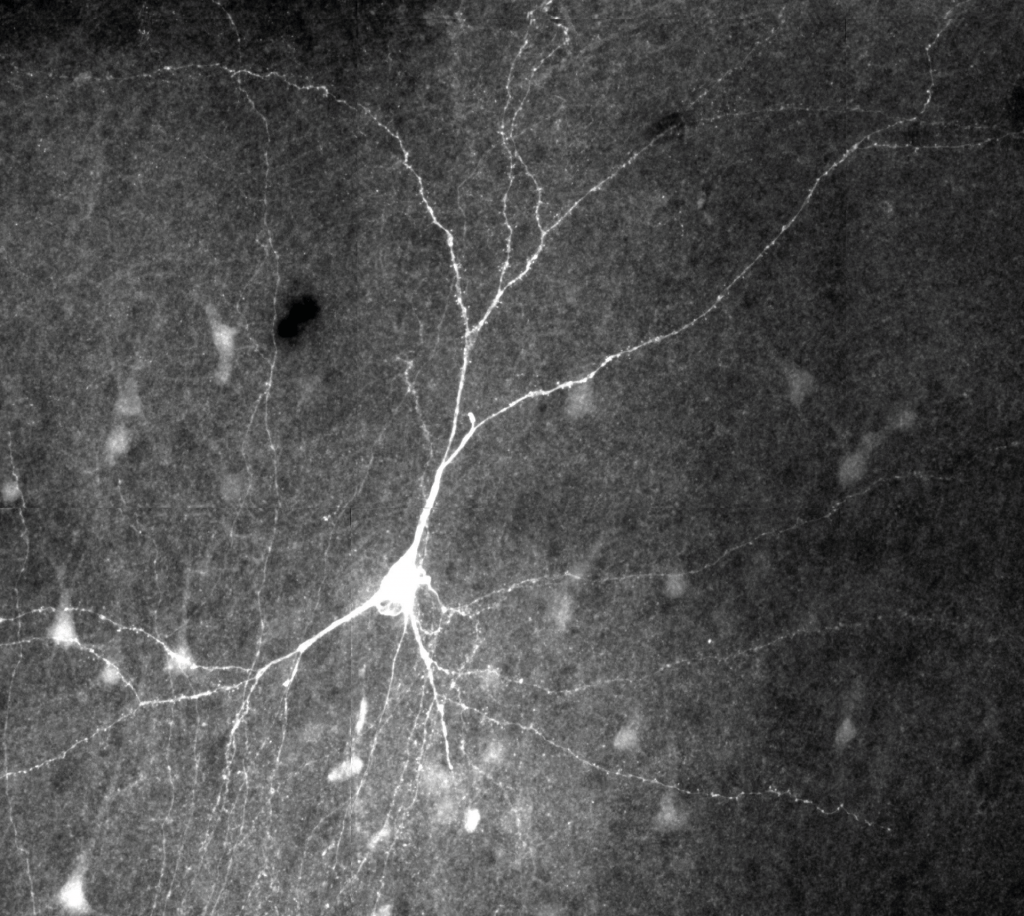
Building on this, in this TIN awarded project, I decided to take advantage of patient-derived models we had previously developed in our lab to assess the efficacy and mechanism of action of combining a P53 reactivator with Photodynamic Therapy (PDT), a light-based therapy which promotes ROS overproduction. I anticipate this strategy will exert a synergistic anti-tumour effect leading to oxidative damage and cell death of mtp53-harbouring cancer cells. The RNA-sequencing and efficacy data derived from this project will be used to apply for follow-on funding to move our research project down the translational pathway.
What is the motivation behind your project/therapeutic?
Pancreatic cancer is the 5th most deadly cancer worldwide (~432,000 deaths/year) and is projected to rank 2nd by 2030. PDAC outcomes are very poor (5-year survival rate <9%) and mtp53 expression correlate with poor prognosis. Adjuvant treatment with gemcitabine following surgery is the standard of care, however, <20% of patients are found eligible for surgery. Aggressive chemotherapy combinations, restricted to fit patients, only marginally improve outcomes so novel therapeutic strategies are urgently needed. Using a therapeutic strategy that restores the tumour suppressor functions of mtp53, and induces oxidative stress (ROS), has the potential to kill cancer cells. However, this strategy for PDAC therapy remains underexplored.
Considering the limited benefits provided by current treatment options, the variety of dysregulated signalling pathways in PDAC, and that mtp53 confers chemotherapy resistance, targeted and combination therapies hold potential to improve patient outcomes. I propose a novel approach to synergistically target the impaired antioxidative response of cancer cells, inducing extensive cell death. I expect the proposed combination to be more effective than chemotherapy alone, with significantly less systemic side effects, enabling treatment of less fit patients.
Can you highlight any challenges you have experienced as an early career researcher in the repurposing/translational research space?
As an early career researcher in the translational research field, obtaining funding to perform your own independent research is challenging and usually requires having preliminary data already available. Gaining access to patient-derived samples can also be a tricky and slow process. I could also say, surviving in academia as an early career researcher, without a permanent position is on its own, a big challenge! I have also found it challenging to develop a network of collaborators and partnerships, particularly with industry. Moreover, understating the complexity of the translational research pathway, including intellectual property (IP), and developing an entrepreneurial mind set, requires specific training.
Why did you want to apply to the Repurposing TIN Pilot Data Fund?
I had obtained some preliminary data supporting this project, but which needed further validation. The Repurposing TIN Pilot Data Fund therefore was the perfect scheme to take this work forward, while also allowing me to lead and manage a grant from scratch, fostering my career development, and supporting my career goal of becoming an independent investigator. I expect data derived from this project will attract follow-on funding to accelerate our research project into the next phase in the translational pathway.
Join the Repurposing TIN
How did you find the process for the TIN Pilot Data Fund?
I think the guidelines were detailed and clear. The application process was well-organised, with excellent communication from the TIN Pilot Data Fund team, of which I am very grateful for the help throughout the process. I also truly appreciated the constructive feedback and advice provided by the committee.
Learn more about the support provided through the TINs
The ACCELERATE training programme has been very important in my translational progression – I think I have attended the majority of the workshops! Prior to the submission of my application, I particularly valued the seminars on IP, Entrepreneurship Skills for Researchers and ‘Grant Writing and Data Management for Translational Research’. Additionally, the pitch coaching we received was key to winning the award.
What do you hope to achieve in the 6 months duration of your project?
In this proof-of-concept study, I plan to evaluate the potential of a p53 reactivator in combination with a ROS-mediated therapy as a new therapeutic strategy for pancreatic cancer, using patient-derived models available in the lab. The resulting RNA-sequencing data will improve our understanding of the mechanisms underlying PDAC vulnerability/resistance to therapy and identify new therapeutic targets. I hope this study will constitute the foundation for subsequent grant applications to move the project closer to clinical translation.
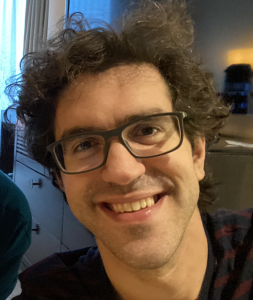
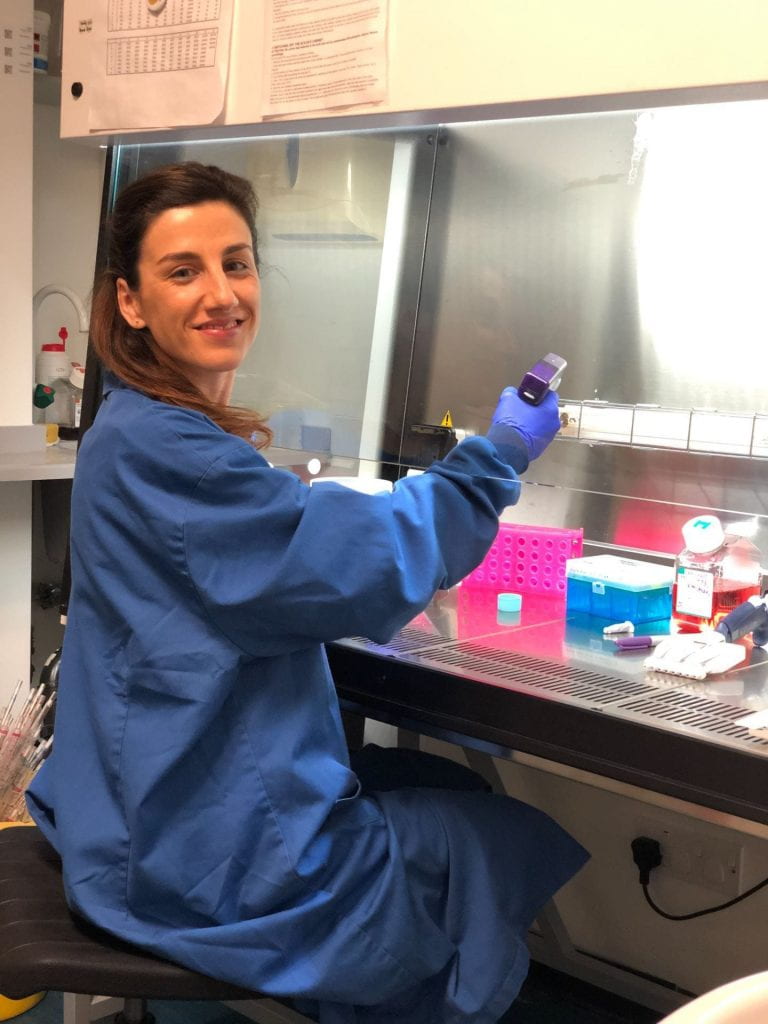
About Dr Pilar Acedo

Dr Pilar Acedo, is a Senior Research Fellow at the UCL Institute for Liver and Digestive Health, in the Division of Medicine, based at the Royal Free Hospital campus. After receiving her PhD in Genetics and Cell Biology from the Autonomous University of Madrid (Spain), Pilar held a postdoctoral position at the Karolinska Institute (Sweden), before joining UCL in October 2015.
Her current research aims to generate patient-derived cancer models as preclinical tools to study disease progression and to predict treatment response. Pilar investigates novel combination therapies to treat pancreatic and bile duct tumours, using nanomedicine and light-based therapies. Her research interests also include the development of biomarkers and imaging tools for the early detection of pancreaticobiliary cancers, using non-invasive approaches (Follow Pilar on Twitter: @pilar_acedo).
 Close
Close