Early Career Innovators: Personalised Therapy for Prostate Cancer from Diagnosis, Devices & Diagnostics TIN
By Alina Shrourou, on 4 February 2021
In the first Devices & Diagnostics TIN interview as part of the Early Career Innovators series, acknowledging the amazing translational work being done by early career researchers within the UCL Therapeutic Innovation Networks (TINs), Dr Hayley Pye highlights her Devices & Diagnostics TIN (co-lead by the UCL Institute of Healthcare Engineering’s Translational & Industry Delivery Group) Pilot Data Fund awarded project, “Personalising pathology for prostate cancer, a unique opportunity at UCL/UCLH”.
What is the title of your project and what does it involve?
I was recently awarded money from UCL TRO’s Therapeutic Innovations Network, specifically the Devices & Diagnostics TIN, to carry out some proof on concept work predicting molecular pathways from diagnostic histology images. The project is called: “Personalising pathology for prostate cancer, a unique opportunity at UCL/UCLH.”
Prostate cancer is the 2nd most common cause of cancer death in males in the UK with over 11,000 men dying each year. Around 350 people are diagnosed with prostate cancer every day. In the UK there are no molecular profiling tests recommended for risk profiling or treatment selection. Despite high quality research in this area, molecular tests to diagnose only the more aggressive cancers that require treatment are largely unadopted. Our device will provide a completely novel way to implement personalised diagnosis and pave the way for the implementation of these tests.
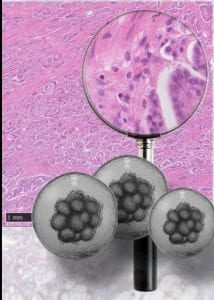
Every cancer diagnosis requires the analysis of a histopathology image, this image (right) is produced from staining a human tissue sample with two dyes (hematoxylin and eosin).
I want to apply machine learning techniques to these whole-slide-images (WSI) and predict for clinically actionable genetic mutations or pathway activation in prostate cancer. This would promote personalised therapy from the point of diagnosis.
Our network provides a unique environment to test this in clinical hands and in real life clinical data sets that are relevant to the target population.
What is the motivation behind your project/therapeutic?
Traditional ‘one size fits all’ treatments for prostate cancer can cause a lot of off target urinary, sexual and bowel symptoms, and overtreatment is common. Our device ultimately will be pathway to implement augmented filters that would overlay an individual’s standard of care diagnostic whole-slide-images (WSI) and inform the patient if they could be spared treatment and/or if a modern targeted treatment could work. This device would help introduce molecular profiling at diagnosis (not yet standard of care) and therapy choice based on the individual cancer’s molecular characteristics.
The diversity in molecular characteristics present in prostate cancer means simple molecular signatures often either struggle to predict treatment sensitivity accurately, or are not present in sufficient numbers of patients. In depth genetic and transcriptomic sequencing can provide comprehensive information about individual tumours but it is expensive, requires the destruction of tissue samples, and the time to result can be long. The translation of in depth genetic and transcriptomic sequencing tests into clinical implementation is challenging due to issues of scale, as well as financial and infrastructural limitations in many centres. The ubiquity of the ‘standard of care’ histopathology slides alongside our device would allow for quick and cheap pre-screening of patients and without any additional tissue.
Why did you want to apply to the Devices & Diagnostics TIN Pilot Data Fund?
Since I am a postdoctoral research associate, the opportunities to raise money and lead your own research project are rare and competitive. However they are also essential if you want to continue a career in academic research. These opportunities are especially challenging as it all has to be done on top of an already busy and challenging day job as a research associate. The TIN Pilot Data Fund is perfectly sized and suited for an opportunity to carry out some independent research within my current role at UCL. In addition, the amount of support and guidance is phenomenal, ideal for someone like myself trying to make that first step into independence.
Learn more about TIN opportunities for researchers
How did you find the process for the TIN Pilot Data Fund? What did you learn?
I felt very supported and encouraged throughout the process. I am still learning and hoping to take advance of all that ACCELERATE can provide, they are very approachable and all the content so far has been appropriate and all very reasonable and relevant. I have attended the following courses: ‘Mentoring for Medical Innovation’, ‘Grant Writing for Translational Research’ and a ‘Pitching Skills Workshop’ as well as applying for a ‘Dragon’s Den’ style grant from the Devices & Diagnostics Therapeutic Innovations Network.
Register for upcoming ACCELERATE events
What do you hope to achieve in the 6 months duration of your project?
Funds from this grant will help to progress a proof of concept computer algorithm through to testing on real-world diagnostic data. Work will involve curating and cleaning the cohort(s) for this type of work, building a strong hypothesis on which to build a model, generating molecular label data for the test cohort, designing suitable approaches for the data pipeline, and finally applying at least one algorithm to real-world diagnostic data. Hopefully I will then be in a strong position to apply for further funding, leveraged by this work, to both access a larger clinically relevant biobank, expand the algorithms to other molecular signatures and embed our tools into a commercial platform already embedded for NHS-wide deployment.
What are your next steps from now?
The most difficult and time-consuming task will be generating reliable and high-quality molecular label data. So this is my main focus at the moment.
About Dr Hayley Pye
Dr Hayley Pye is a Postdoctoral Research Associate based in the Division of Surgery at UCL. She is currently working on a clinical trial evaluating new blood and urine biomarkers in combination with MRI imaging for improved prostate cancer diagnosis and prognosis. She also has experience in the early-stage development of antibody-drug conjugates (ADC) that can be activated by light (photodynamic) sound (sonodynamic) or carrying chemotherapeutic drugs for cancer.
She is driven to better understand the way we currently diagnose and choose modern therapeutics for cancer in the clinic and wants to disrupt the stratification by ‘organ of origin’ and the research silos we currently work in.
 Close
Close