Fibreless Diffuse Optical Tomography summer internship
By rmapapg, on 31 October 2018
by Aman Ganglani
Over the summer I was lucky enough to be given a leading role in an 11 week research project working with Dr. Robert Cooper, Dr. Hubin Zhao and Dr. Sabrina Brigadoi on a fibreless Diffuse Optical Tomography (DOT) system.
DOT is a novel imaging technique that has a wide variety of applications in neuroscience and clinical research. Specifically, using DOT to investigate neonatal brain development is a very important focus. Cerebral haemodynamic patterns in brain injured neonates is not well understood. Complications at this vital stage of development can result in critical danger to the patient and long-term disabilities. Further investigation into these complex haemodynamic signals is necessary to better understand the underlying physiology and to develop DOT into a novel imaging tool that could help diagnose and treat compromised infants [1].
Current DOT technology is limited by bulky fibres which limit comfort, movement and ease of use. Transforming the current DOT systems into wearable, fibreless devices is a vital step in the development of DOT technology [2]. This advance will enable long term clinical application of DOT, improve data quality and make the instruments viable in a wider range of applications. However, transforming the bulky wearable DOT modules into a fibreless wearable comes with challenges. This investigation aimed to minimize motion artifacts with fibreless systems. While there are post processing methods of tackling motion artifacts [3], they alone are not enough for fibreless systems. Our novel approach has been to develop the application of motion sensors specifically for this type of movement and add them to the current fibreless systems to build the world’s first dataset of fibreless DOT and 9 axis (3x accelerometer, 3x gyroscope and 3x magnetometer) motion data.
We decided to focus our investigation on the effect of forced induced movement on DOT data. We introduced two 9 axis motion sensors along with 2 DOT fibreless modules each containing a 9 axis motion sensor. Our experiment paradigm consisted of controlled head, eyebrow and full body movements.
After many considerations, we purchased two Razor 9DoF motion sensors containing the MPU_9250 Invensense chip which is the same sensor used on the DOT modules. I was able to match the operating conditions of the chip with the DOT chip by writing my own code in the Arduino IDE and MATLAB. This would ensure data acquired from both sensors could be accurately compared.
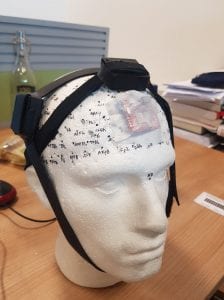
Due to the DOT modules being standalone devices, I also had to figure out a way of mounting everything (the two DOT modules and the two motion sensors) in a comfortable way. After a lot of experimentation and time in the Institute of Making, I managed to build my own headgear system which kept all the sensors completely independent of each other. The DOT modules were secured using separate sewn velcro and rubber band straps while the motion sensors used adhesive tape placed directly on the scalp.
Finally, all this preparation was for the experiment paradigm itself. We eventually decided we wanted to investigate the effects of eyebrow movement (this has not been explored and previous pilot studies showed large eyebrow related artifacts), the effect of scalp movement compared to head movement and induced head movement along with walking and designed a paradigm accordingly.
Within each block, chirp noises of decreasing lengths were used. When the subject hears the chirp, they must move their head throughout the chirp, this way we can control the speed of movements. Varying the speed of these movements is useful because is allows us to look at relationships between the sizes of motion artifacts and the speed of movement. The speaking section was done with words of varying syllables for the same reason. The timing of eyebrow movement was controlled by a simple tone sound rather than a chirp, because it is difficult for people to control the speed of eyebrow raises.
Additionally, I created a MATLAB script which would efficiently run everything with one press of a button using parallel computing. This massive streamlining of the whole experimental procedure will make studies synchronised and far easier to run. Our aim in the first term is to use my experiment to run multiple studies on a variety of healthy adult volunteers.
Our initial conclusions show that more investigation into 9 axis data with fibreless systems is clearly justified. I was able to help publish a poster which was presented at the fNIRS 2018 conference in Japan titled ‘Investigating the Benefits of Integrated Motion Sensing and Wearable, Modular High Density Diffuse Optical Tomography’, of which I was an author.
This has been an incredible experience. In 11 short weeks, we have managed to build and execute an experiment paradigm which has never been done before. I have been exposed to real research and have obtained a publication under my name by having my work presented at a conference. I will continue to work with the team throughout the first term.
I would like to thank Dr. Zhao, Dr. Brigadoi and Dr. Cooper for their never-ending patience and commitment. They have exposed me to world-leading research and have given me an excellent insight into the life of an academic.
1 Cooper RJ, et al. Transient haemodynamic events in neurologically compromised infants: a simultaneous EEG and diffuse optical imaging study. Neuroimage (2011).
2 Danial Chitnis, et al. Functional imaging of the human brain using a modular, fibre-less, high-density diffuse optical tomography system. Biomed Opt Express. 10 (2016)
3 Cooper, R. J. et al. A Systematic Comparison of Motion Artifact Correction Techniques for Functional Near-Infrared Spectroscopy. Front. Neurosci. 6, (2012)
 Close
Close