“You, me and the Big D”: Changing attitudes to dementia in Whiteley Village through participatory research
By rmjlmcd, on 18 September 2019
In this post, Rachael Frost talks about her experience of conducting a participatory research project.
Whiteley Village is a retirement community in Surrey for people on low incomes. Dating back to 1917, the village provides housing, support and facilities for nearly 500 older people. Managed by the Whiteley Homes Trust, the village can support those with care needs in assisted living or a care home, but there are no dedicated dementia facilities. Despite this, a number of residents are living there with varying degrees of dementia. Although the village has a strong sense of community and residents can be very supportive towards each other, there is a sense that dementia is still stigmatised like cancer used to be (the old “Big C”) and that as a result, residents don’t receive the support they could from each other.
Enter Pauline, Mary, Peggy and Sue – four village residents who wanted to change this. In partnership with Dr Alison Armstrong from the Whiteley Foundation for Ageing Well and myself, we successfully applied for a British Society of Gerontology Averil Osborn Award for Participatory Research at the end of 2018.
The “You, Me and the Big D” project was a small research project designed to see whether Alzheimer’s Society Dementia Awareness Training would have a positive impact upon residents’ attitudes and behaviours to people in the village with dementia. Mary, Peggy, Pauline and Sue collected qualitative and questionnaire data from eight participants before and after the training, with qualitative research training and input throughout from Alison and myself.
So did anything change? Before the training, our participants told us that although they knew how to best support someone with dementia, they had plenty of examples from the village where this hadn’t happened. They felt this was due to lack of knowledge, village life (which could be supportive but judgmental), fear and the fact that different people with dementia had very different symptoms. Participants felt there was a need for more village support and wanted more information, particularly about dealing with aggressive behaviour.
“One day they might seem perfectly normal to you and the next day they’re not” (Barbara)
After the training, our eight participants felt like they had learnt quite a lot about different types of dementia and its other effects (such as on the senses and on balance), but wished to know a lot more than could be covered in three hours. For a couple of participants, it increased the worry about potentially aggressive behaviour from people with dementia. Some participants also reported issues with the training facilitation in that they would have liked to hear more from the speaker than others in the room.
“I’ve learned that there are different types of dementia which I hadn’t really considered and … people who have dementia are at different stages” (Camilla)
It was a great project to be involved in, although there were some challenges along the way! There was very little time to actually do the project (we received confirmation of the funding in January and had to present results at the British Society of Gerontology conference in July), particularly for training in qualitative interviewing and analysis, and very little budget. Some of the villagers weren’t receptive to the idea of other villagers doing research – with people saying “who do you think you are?” According to the village researchers, confidentiality was also a challenge in such a closed environment, as was having audio-recorders that were not very older person-friendly!
However, the benefits definitely outweighed these. Alison and I had a great time as the village researchers were so enthusiastic. Peggy, Mary, Sue and Pauline looked forward to our meetings and discussions, enjoyed learning and making a difference to the village and said they felt younger as a result. Mary and Sue came along to British Society of Gerontology 2019 conference and co-presented the project with Alison.
Of course, this was only a very small project. However, the main positive benefit from the Big D has been its wider impact on the village. Whiteley residents have been encouraged to talk about dementia more and dementia care has moved up the agenda with management. One person with dementia has even been able to move back into the village and live back with their spouse with better support. Further projects are being planned to improve dementia support in the village, so watch this space…
Accessing GP appointments- a disaster waiting to happen or hope on the horizon?
By Nathan Davies, on 16 May 2019
In this post Ruth Abrams and Sophie Park reflect on the current pressures facing GPs and NHS today.
In a recent expose called ‘GPs: Why Can’t I Get an Appointment?’, a Panorama documentary, which aired on BBC1 on Wednesday 8th May, emphasised the current limits of and pressures on the NHS system. The programme featured interviews with overworked GPs and allied healthcare professionals, painting a rather bleak picture. Practices are merging and closing at an ever increasing rate. Patient loads increase as patient lists are subsumed. Patient multi-morbidities have increased the need for chronic conditions to be monitored with regular GP appointments. Yet on average patients wait a minimum of two weeks for a routine appointment. Early retirement and a limited flow of trainees into General Practice also contribute to the strain, making practice sustainability difficult to envisage. Inevitably, pressure and frustration are being felt amongst both patient groups and the primary care workforce.
Whilst those researching, working in and experiencing primary care within the UK will already be familiar with these factors, what has become a pressing concern since the 2015 publication of the BMA’s, National survey of GPs: The future of General Practice, is patient safety. At present only the most urgent of cases are seen quickly in General Practice. Yet still an unsafe number of patients are seen by any one GP in a day. This high demand placed upon GPs makes for little time to reflect on cases.
Enter- the release of the new GP contract and the NHS long term plan which intend to employ a multi-disciplinary army of healthcare professionals. Within this new way of working, workloads will be shared amongst staff, with greater efforts being made for both integration and collaboration. A typical GP’s day will begin to look very different. Micro-teams will have time to discuss patient cases, a GP’s time can once again be focused on the professional tasks only they can undertake and overall there begins to be a healthier outlook to teamwork.
Some promote this utopian vision of General Practice working unquestioningly. Pots of money, such as those made available through the Prime Minister’s Fund, have encouraged new ways of working with very limited evidence base. Yet one aspect seemingly unaddressed within the new plans is the disparity across patient access and levels of deprivation within the UK. In a recent report by the Health Foundation, GPs working in higher deprived areas see more patients compared to their counterparts. These are areas where recruitment of this new workforce will inevitably be harder. This raises questions about how best to incentivise recruitment so that patient access to care remains equal for all.
There is also a certain feel that these plans are being done to, rather than with GPs. We need only reflect back a few short years to the junior doctor protests to recall that in order for patient safety to happen, workforce perspectives must be accounted for. In order for the NHS to remain as successful as it has been and for the principles of Astana declaration to be realised, GP engagement rather than negation needs to remain central to all future planning activities.
Unequal access to care and a disruption to professional identities present major issues. But doing nothing is no longer an option. At a time when the NHS is so often synonymous with the words crisis and strain rather than success, a Utopian vision for both staff and patients may be both timely and necessary. Reifying this however, becomes a different matter all together.
The unexpected consequences of researching unexpected consequences: The DECODE Study
By rmjlmcd, on 15 March 2019
In this post, Lorraine McDonagh, Sarah Blake, Fiona Stevenson, and Fiona Hamilton (on behalf of the DECODE study team) reflect on the unexpected consequences of researching unexpected consequences.
 The DECODE (UnexpecteD Consequences Of Digital hEalth Tools) Study aims to explore the unexpected consequences (both positive and negative) of digital health technologies for patients, GPs and general practice staff. We are particularly interested in smartphone apps, online consultations with GPs, and patients having online access to their medical records. The project is funded by the NIHR School for Primary Care Research.
The DECODE (UnexpecteD Consequences Of Digital hEalth Tools) Study aims to explore the unexpected consequences (both positive and negative) of digital health technologies for patients, GPs and general practice staff. We are particularly interested in smartphone apps, online consultations with GPs, and patients having online access to their medical records. The project is funded by the NIHR School for Primary Care Research.
Late last year, we ran a workshop with members of the public/patients, researchers in the field, technology developers, and GPs to help identify areas we should be thinking about when considering the unexpected consequences of using digital tools in primary care. The findings of this workshop are discussed elsewhere, but here, we reflect on the unexpected consequences of researching unexpected consequences.
Before
Setting-up the workshop proved more challenging than expected. We wanted to have equal numbers of people in each of our key stakeholder groups – patients, researchers, technology developers, GPs and practice managers. Accessing researchers and GPs interested in this topic was reasonably straightforward – possibly because most members of the DECODE team fit within one of these groups! However, we didn’t manage to recruit any practice managers, despite repeated emails and phone calls, keeping in mind that attendance was voluntary. We put a lot of effort into seeking out technology developers, we even signed-up for a Premium LinkedIn account and contacted developers directly but no one responded. Eventually, after exhausting all our contacts and trawling the internet, four technology developers agreed to come.
During
We planned to organise attendees by profession into mini-discussion groups, but on the morning of the workshop, three technology developers could not make it and had to drop out. We learned the one technology developer who turned up also had research experience so we decided to pair him with the researcher group. Unexpectedly, we soon learned that many people in attendance had multiple roles and could bridge across several of our pre-defined groups – for example, one patient was an ex-GP, one PhD student researcher was also a GP, and the technology developer was also a former GP.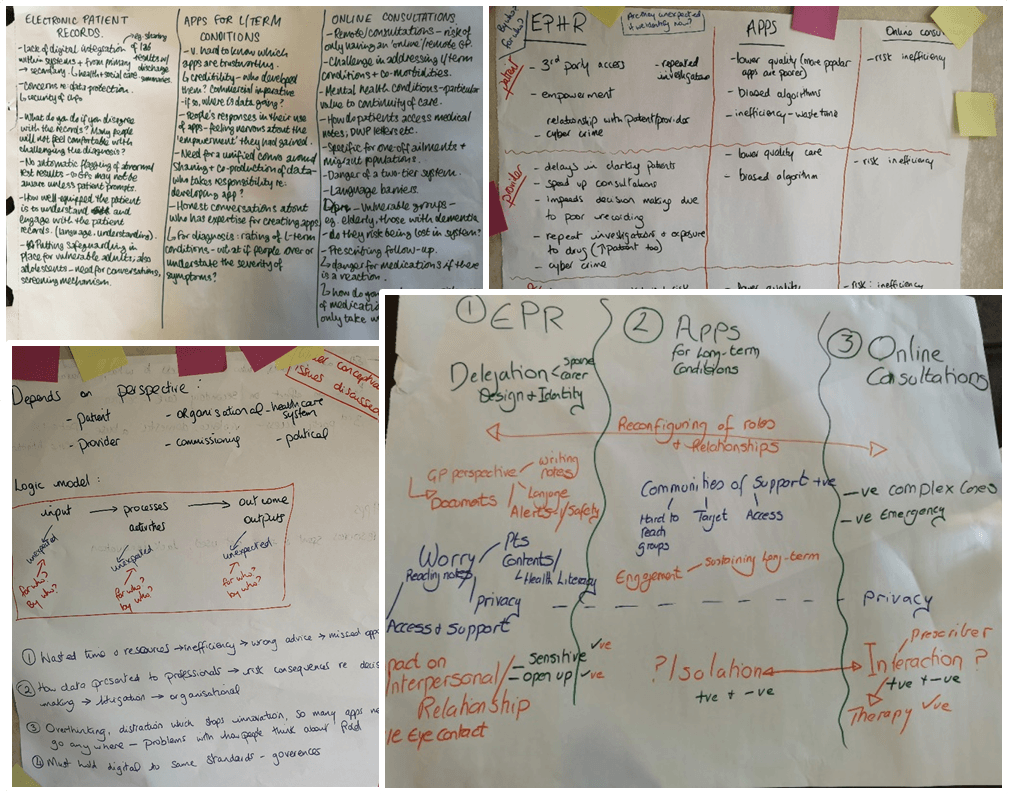
Importantly, not all unexpected consequences are negative; we gained more insights than expected. For example, one GP gave an impromptu presentation of how well his practice has been using digital tools. At points, different competing priorities among the diverse stakeholder groups were evident, with some interested in the practical unexpected consequences, such as data security (the patient and GP group), and others keener on theoretical standpoints (the researcher group). To illustrate, one task was to discuss what potential unexpected consequences could occur from use of apps, online consultations, and patient access to electronic records. The researcher group felt that this required a literature review and directed their discussions towards devising a logic model for understanding unexpected consequences. The other groups, however, as anticipated when devising the task, drew on, presented and discussed their own experiences of digital health technologies.
Some members of the patient group were concerned about changes resulting from the increasing use of digital health technologies. Unexpectedly, the greatest ambition of these patients was to use digital tools to feel a sense of empowerment and autonomy in consultations and healthcare provision. They spoke negatively about paternalistic attitudes from clinicians and wanted to move towards  more equal partnerships and involvement in decision making regarding their health. They felt this could also increase their safety and well-being, as technology would enhance their ability to self-monitor health. It is important to remember that these patients, who gave their time to share their views, are not necessarily illustrative of how every patient would feel. Some patient/public views remain absent from research, despite efforts to bridge these gaps. There are many reasons patient/public views can go unheard; people may be inaccessible due to vulnerability (e.g., those who are homeless, those with learning difficulties, those with languages other than English), or simply by being too busy to be heard (e.g., those with substantial caring responsibilities, those in full-time employment). Building an inclusive picture of patient/public voices remains challenging.
more equal partnerships and involvement in decision making regarding their health. They felt this could also increase their safety and well-being, as technology would enhance their ability to self-monitor health. It is important to remember that these patients, who gave their time to share their views, are not necessarily illustrative of how every patient would feel. Some patient/public views remain absent from research, despite efforts to bridge these gaps. There are many reasons patient/public views can go unheard; people may be inaccessible due to vulnerability (e.g., those who are homeless, those with learning difficulties, those with languages other than English), or simply by being too busy to be heard (e.g., those with substantial caring responsibilities, those in full-time employment). Building an inclusive picture of patient/public voices remains challenging.
After
The key lesson we’ve learned from this experience was the power of combining individuals across key stakeholder groups. However, we are left wondering what voices have we missed? How do we know the unknowns? To shed further light on these issues, our colleagues at University of Oxford are conducting a conceptual literature review and colleagues at Universities of Bristol and Manchester are conducting interviews with patients, primary care staff and technology developers. Following on from which, we (the UCL team) will be carrying out another workshop with stakeholders.
The team is also keen to get as many views as possible on potential unexpected consequences of digital technology. If you have any insights related to these three types of technology or would like to comment on the unexpected consequences identified so far, please contact Andrew Turner or take part in Twitter discussions using the hashtag #DECODEstudy.
Health indicator recording in UK primary care electronic health records: key implications for handling missing data
By Nathan Davies, on 13 March 2019
In this post Tra My Pham talks about their latest paper which has investigated the recording of data in UK primary care electronic health records and the implications this has on conducting research using these records.
GP electronic health records provide a large amount of information and data for medical research. These information source help us to study individuals’ health over time, and offer many opportunities for research into populations that would otherwise be difficult and/or expensive to undertake.
Large UK primary care databases (GP electronic health records) capture information on key health indicators such as height, body weight, blood pressure, cholesterol level, smoking status, and alcohol consumption. These are relevant risk factors for many health conditions including diabetes and heart diseases, which remain leading causes of the global disease burdens. In primary care when patients register with their GP practices, it is typical that their past and current medical history is documented. Most individuals will have a record of the above health indicators as part of their registration. Thereafter, this information is mainly recorded if it is directly relevant to the patients’ care, ie, some patients will have several records over time while other will only have a few. Therefore, data can often be incomplete, which poses a challenge for their use in research. In this study, we aimed to further understand how common health indicators are recorded in the UK primary care setting, and whether there are potential implications for dealing with incomplete data in medical research.
We analysed records of height, body weight, blood pressure, cholesterol level, smoking status, and alcohol consumption from 6.3 million individuals aged 18–99 in The Health Improvement Network (THIN) database during the period 2000–2015. There were differences in the recording of these health indicators by sex, age, time since registration with the GP practices, and disease status. In particular, women aged 18–65 years were more likely than men of the same age to have these health indicators recorded, and this gap narrowed after age 65 (Figure 1). More than 60% of individuals had their health indicator data recorded during the first year following registration with their GP practices. After that, this proportion fell to only 10–40%. The recording of relevant health indicators were more regular among individuals with chronic diseases compared to those without, eg, body weight being measured more frequently for diabetes weight management (Figure 2).
Health indicator recording in general practices followed, to some extent, the GP consultation patterns by age and sex. In particular, younger women were more likely to see their GPs than younger men. Therefore, it seemed likely that for women, many weight and blood pressure measurements may have been taken in conjunction with their consultations for contraception and pregnancy. Our results suggested that many practices offered general health checks for their newly registered patients, during which patients’ health indicators were recorded. A GP incentive scheme was introduced in 2004, under which GPs receive financial payments based on quality targets and they have to record data, eg, health measurements, in order to meet these targets. Since this scheme began, many individuals with chronic conditions have had their health indicator measurements recorded on a more regular basis, which was reflected in our findings.
For health research studies using primary care databases, incomplete information on common health indicators will affect statistical analysis. In particular, analyses based on the available information alone may be misleading. It is standard in medical research to overcome the problem of incomplete data by using a statistical method called multiple imputation. The method involves using the data collected to estimate the unseen data (several times for each unseen value), so that analysis can proceed as though complete data had been collected. Based on the findings of our study, multiple imputation taking into account the differences in health indicator recording by individuals’ demographic characteristics and disease status is recommended, but should be considered and implemented carefully.
Our article and relevant references can be found at:
Petersen I, Welch CA, Nazareth I, Walters K, Marston L, Morris RW, Carpenter JR, Morris TP, Pham TM (2019). Health indicator recording in UK primary care electronic health records: key implications for handling missing data. Clinical Epidemiology, 2019 (11) pp. 157-167. https://doi.org/10.2147/CLEP.S191437.
A design for life –Finsbury health Centre- a forerunner for NHS primary care
By Nathan Davies, on 3 December 2018
In this post Melvyn Jones talks about how the iBSc in Primary Health Care students visit a local GP health centre and learn about who it was developed to meet the needs of it’s patients on the eve of World War II. 
The words of a 1940s poster “fight for it now” and its gleaming image of Finsbury Health Centre directly linked fighting during that recent conflict with needs of soldiers and a beleaguered population for a better life after World war 2. The pre NHS Finsbury Health Centre which opened in 1938 on the eve of war, offered a model of community based health care away from the hospitals, to meet the needs of its very deprived population; burdened with poverty, malnutrition, lice, TB and rickets.
Roll forward nearly 80 years and the current batch of iBSc in Primary Health Care students were shown how this building was designed to meet the health needs of that time; with lead lined walls for the TB x-ray screening service, the solarium was there to prevent rickets and the layout was designed to help clinicians provide the best care they could (the corridors are bright and diamond shaped to encourage interaction between staff). Dr Marie de Souza, one of the GPs working in the practice discussed how in some ways they are still using this building to deal with similar issues (communicable disease like HIV, vitamin D deficiency due to poor diet and lifestyle) and some issues we still can’t seem to address- we were shown the reception rooms in the basement where homeless families were temporarily housed. Yet there are newer challenges like the increasing burden for people with poor mental health. Rooms that once were used to de-louse bedding are now used to provide CBT. There are considerable constraints involved in providing 21st century health care from this grade 1 listed building (Lubetkin’s architectural master piece). A repair must look like an unsightly repair (so the building can be “read” by the streams of architectural students), a picture can’t be hung without permission from English Heritage, the door locks can’t be updated because the lead walls are indestructible. And yet, today on a sunny November morning, the light flooded in through the expanses of glass; glimpses of that gleaming 1940s image of hope.
The students were encouraged to think how they might shape the health service for the next 80 years and how the buildings we might get to design could reshape the care we could provide.
Case management pro lidi žijící s demencí a jejich rodinné příslušníky
By Nathan Davies, on 11 October 2018
Jane Wilcock & Steve Iliffe , Centre for Ageing Population Studies
For the last few years we have been collaborating with colleagues from the Centre of Expertise in Longevity and Long-term Care, Faculty of Humanities, Charles University in Prague, Czech Republic. The Ministry of Health of the České Republiky tasked us with exploring case management as a complex intervention in people with dementia. A multidisciplinary team with experiences in general practice, sociology, nursing, ethics, social care and psychology led by Iva Holmerová, we set out to explore the current understanding of dementia case management and develop a toolkit for implementation in the Czech Republic, where no such model currently exists.
In Europe people with dementia syndrome and their carers all too often encounter services that are limited in resources, poorly coordinated, variable in quality and quantity, protocol-driven, inequitable, sometimes stigmatising and are only weakly tailored to individual and family needs. These negative features appear common across Europe, where there is a need to develop new (or reconfigure existing) services for people with dementia and their families so that they experience a smoother journey along the illness trajectory and receive services that are more person-centred, effective and efficient. One strategy for improving the effectiveness of care is to develop programmes that enhance coordination and implementation of care plans.
Through a series of workshops with key stakeholders, literature review and ethnography we modelled case management for dementia which led to a discussion paper in the International journal of Dementia, several Czech monographs, a toolkit of skills for dementia case managers and a guide to good practice in implementing case management.
In September I was invited to present a half day workshop on case management for people with dementia at the Gerontological conference in Prague co-hosted by the Czech Alzheimer’s society in the impressive National Technical Library. The workshop was well attended, we had a mix of nurses from care homes and social workers and their managers. English was not widely spoken by the attendees and it was a new experience for me having my words translated into Czech and then the questions and lively discussion translated back to me in English.
The following day I was invited to present on case management at a workshop in the district of Prague 7 where they want to implement case management across all sectors. It was an informal afternoon in a local café and was attended by commissioners, social workers, housing and representatives from the third sector such as the local YMCA and the Salvation Army. Complex caseloads of people who are homeless, those with drug and alcohol problems as well as those with dementia, led to the interest from practitioners. The end of the workshop led to some practical definitions and ways forward for implementation, and was a rewarding process to be involved in.
As our three year collaboration ends this year we are looking for new ways to continue to work together on this successful collaboration. And I am looking forward to presenting research methodologies to the PhD students at the Prague Centre of Expertise in Longevity and Long-term Care in November.
This study was supported by the research project 15-32942A-P09 AZV of the Ministry of Health České republiky Case management as a complex intervention in patients with dementia
“Why am I doing this?!” A reminder.
By Nathan Davies, on 6 September 2018
I have been assured that asking oneself “Why am I doing this?!” is not an experience unique to any one stage of a research career. The key is having a good answer.
At the height of the British summer heat wave, I travelled to Chicago, to give an oral presentation to the Alzheimer’s Association International Conference (AAIC) on a project I’ve joined, funded by the Dunhill Medical Trust, addressing inequality in primary care of people with dementia among UK ethnic groups.
The first phase of the project has already been published in Clinical Epidemiology and found that dementia diagnosis incidence was significantly higher in Black men and women compared to White men and women, respectively, and was significantly lower in Asian women compared to White women. Tra recently wrote a blog on this below. I presented these results along with new results showing inequality by ethnicity in prescribing of certain drugs among patients with dementia.
The presentation itself went smoothly, and I breathed a sigh of relief as I walked off stage. With the nerves and the bright lights out of the way, I was excited to find that a queue of people were keen to talk with me about the project.
Multiple researchers expressed how grateful they were that someone was looking into this area, highlighting that while the demographics of many developed nations are changing, the research has not often kept up. Others wanted to share personal experiences, speaking of the reluctance of family members to seek a diagnosis or medication even as their condition progressed, especially when cultural factors around memory problems and fear of stigma were at play. These conversations made clear that the need to identify inequalities and break down barriers to good quality care was not a problem unique to the UK, but everyone I spoke with reinforced how important it was to see that we’re working on it.
In the midst of Stata code, funding applications, and reviewer comments, we can lose sight of the goal. As researchers, we have the privilege of generating work that can improve peoples’ lives. We can be reminded of that by our Patient & Public Involvement advisors, our colleagues, or a review of the “Impact” section of our own funding application (and hopefully by this blog post). My conversations with a variety of people after my presentation was a wonderful reminder of the goal and impact of this project. I hope you can take a moment today to remember the goal of your work too, because you’re doing this for a good reason!
A comparison of new dementia diagnosis rates across ethnic groups in UK primary care
By Nathan Davies, on 31 August 2018
In this post Tra Pham discusses her recent work with colleagues from the department, Division of Psychiatry and King’s College London on new diagnoses of dementia and the differences among ethnic groups.
Around 46.8 million people worldwide have dementia; this is expected to rise to 131.5 million by 2050. Recent studies have reported stable or declining rates of new dementia cases overtime.
In 2010, members of our department (Rait et al, 2010, BMJ) conducted a primary care database study to investigate survival of people with a diagnosis of dementia, and reported a stable rate of new dementia diagnoses in UK primary care between 1990 and 2007. We know little about the differences in the likelihood of receiving a dementia diagnosis among different ethnic groups. Some evidence has indicated that people from Black and Minor Ethnic (BME) groups present at services (i.e. GP) later in their illness. Therefore, compared with the White British ethnic group, BME dementia patients may have less access to timely diagnosis. This can prevent them from benefiting from early intervention and treatment which may help slow the progression of the disease.
Our recent study reported the overall rate of new dementia diagnoses in UK primary care between 2007 and 2015. In addition, we reported, for the first time, the rate by White, Asian, and Black ethnic groups. Pulling together current best evidence of new dementia cases in the community and the 2015 UK census data, we estimated the proportion of White and Black people developing dementia who received a diagnosis in 2015. Our hypothesis was that there would be a smaller proportion of Black people with dementia who were diagnosed compared with people from the White ethnic group.
We analysed data of 2.5 million older people from The Health Improvement Network (THIN) database. 66,083 new cases of dementia were identified, which corresponded to an increased rate of new dementia diagnoses between 2007 and 2015 (Figure 1).
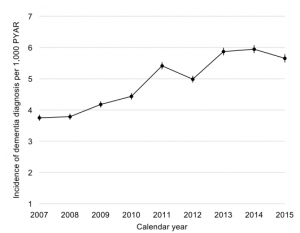
Figure 1 Rate of new dementia diagnoses per 1,000 person-years at risk (PYAR) by calendar year in The Health Improvement Network (THIN) UK primary care database.
Compared with White women, the dementia diagnosis rate was 18% lower among Asian women and 25% higher among Black women. This rate was 28% higher among Black men and 12% lower in Asian men, relative to White men. Based on diagnosis rates in THIN data and projections of new dementia cases from community cohort studies, we estimated that 42% of Black men developing dementia in 2015 were diagnosed, compared with 53% of White men.
The results thus suggest that the rates of people receiving a diagnosis may be lower than the actual rates of developing dementia in certain groups, particularly among Black men. There are several possible explanations for this. It could indicate that Black men experience barriers to accessing health services or receiving a diagnosis. GPs may be more reluctant to diagnose dementia in BME groups especially if culturally competent tests are unavailable. GPs and families might also be reluctant to name dementia in communities where more stigma is associated with a diagnosis.
Our study emphasises the need for service improvement targeting BME groups who might be facing barriers to accessing health care services and getting a dementia diagnosis. GPs should be equipped with culturally appropriate assessment tools in order to make a timely diagnosis of dementia for BME patients.
Our findings also highlight the importance of raising awareness of the benefits of getting a timely diagnosis of dementia, particularly in people from minority ethnic groups who may be more at risk of dementia. Timely diagnosis of dementia can lead to more targeted support and enable GPs to provide appropriate patient care management. These benefits can be explained to the patients by family and friends, as well as professionals such as nurses and social workers. They can also help the patients to overcome the fears of talking about dementia. Faith and community groups can contribute to ensuring that local dementia services are accessible to all.
This study is conducted in collaboration with King’s College London. This work is supported by The Dunhill Medical Trust [grant number R530/1116]. Our article and relevant references can be found at:
Pham TM, Petersen I, Walters K, Raine R, Manthorpe J, Mukadam N, Cooper C (2018). Trends in dementia diagnosis rates in UK ethnic groups: analysis of UK primary care data. Clinical Epidemiology (10): 949-960. doi: 10.2147/CLEP.S152647.
Can a self-management intervention facilitated by peer support workers reduce readmission rates to acute care for people discharged from crisis resolution teams
By Nathan Davies, on 23 August 2018
In this post Louise Marston talks about their recent study published in The Lancet on peer support for reducing readmission among people to acute care for people discharged from crisis resolution teams, which provide intensive home treatment following a crisis.
CORE (CRT Optimisation and RElapse prevention) has been a big part of my working life for a number of years. It was an NIHR funded programme grant from 2011 to 2017. One of the work packages was an individually randomised controlled trial supported by Priment Clinical Trials Unit. The results were published in The Lancet recently.
Why did we do this study?
Crisis resolution teams work in the community to help prevent admission to acute care at times of mental health crisis. Nationally, they have not resulted in a decrease in bed use.
Self-management is a way for people to actively manage a condition; recognising the signs of crisis and knowing how to manage symptoms and other aspects of their life. Interventions may aid self-management, but might be more effective when facilitated and motivated by someone else. Peer support workers have had similar experiences to the people they are supporting, so are able to be a role model for recovery.
Who did we enrol in the study?
We recruited people who had been on the caseload of mental health crisis resolution teams, been discharged from the crisis resolution team in the previous month and had capacity to consent to taking part. We did not recruit those who were deemed to be high risk to them or others, were discharged out of the area or who could not understand English.
What was the intervention?
This was a self-management workbook, which was adapted from other resources in an earlier CORE work package, which was facilitated by a peer support worker in up to 10 sessions. In these sessions, peer support workers were encouraged to help participants complete the workbook and to reflect and discuss their recovery plans. Peer support workers were also employed to provide supportive listening and instil hope of recovery, through sharing strategies to aid recovery learnt through their own recovery journey.
What was the comparison?
Participants in the control group were sent the workbook in the post, but did not have access to a peer support worker and were not given further guidance on how to use the workbook. They could also access usual care.
What did we find?
We found that those randomised to the peer support worker group were less likely to be readmitted to acute care in the year after they enrolled in the study compared with those who were randomised to the workbook alone (29% versus 38% respectively). Time to admission was also significantly longer in the intervention group, as was satisfaction with mental health care and self-rated recovery at 4 month follow-up.
What does this mean?
The rate of readmissions was lower than expected overall. However, peer support workers have the potential to help reduce readmissions further in people who have had a mental health crisis, giving them the opportunity for a sustained recovery. It also means that the burden on acute services will be less; potentially giving savings to the NHS.
Satisfaction with care related to all mental health services; even so as this was statistically significant at four month follow-up suggesting that participants liked having a peer support worker, and uptake of the peer support worker intervention was good. If peer support workers after mental health crisis were more widely available, this may go some way to improving Trust satisfaction ratings.
Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, Ambler G, Milton A, Davidson M, Christoforou M, Sullivan S, Hunter R, Hindle D, Paterson B, Leverton M, Piotrowski J, Forsyth R, Mosse L, Goater N, Kelly K, Lean M, Pilling S, Morant N, Lloyd-Evans B (2018) Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial Lancet 392 409-428 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31470-3/fulltext
Inter-professional working at the frontline; lessons learned from integrated care teams in Tower Hamlets
By rmjlmcd, on 10 August 2018
In this post, Mirza Lalani discusses his experience as an embedded researcher in Tower Hamlets
‘The process whereby members of different professions and/or agencies work together to provide integrated health and/or social care for the benefit of service users’ (Pollard et al, 2005)
Why inter-professional working? The World Health Organisation (WHO) has stated that inter-professional collaboration is an essential component in satisfactory service delivery.
Health and social care systems in the UK are facing unprecedented pressures to manage rising demand from an ageing population, which is compounded by an increasingly demotivated and constrained workforce and the requirement to operate within tight financial parameters. Integrated care is often presented as part of the solution, as strengthening coordination between health and social care systems and among different care settings to provide joined up care that can help meet the needs of the growing number of patients with complex health and social care problems.
In 2015, the NHS England Five Year Forward View put a lot emphasis on new models of care based on the idea that care should be person-centred. One of these new models of care, a Multi-specialty Community Provider (MCP) partnership of health, social and voluntary care providers and commissioners in Tower Hamlets, was awarded Vanguard status in 2015. A key aspect of the Vanguard programme is inter-professional working, especially between frontline health and social care professionals with the goal of providing holistic care.
For the last 12 months, I have been working as an embedded researcher in Tower Hamlets spending a lot of time with frontline multi-professional teams to understand how they work. These teams include community nurses, physiotherapists, occupational therapists, care navigators and social workers working together to meet patients’ needs in their locality. The co-location of these staff is an important step towards integration, but its impact is often overstated and in reality professional culture, identity and boundaries make it difficult for senior management to realise their vision of a fully integrated, coherent and joined up health and social care service. For instance, having different management lines (for social workers on the one hand and health professionals on the other) can be a barrier to people feeling like they belong to one team.
There are some reasons to be optimistic. I have witnessed a cultural shift among health professionals, in particular GPs, who are more inclined to refer patients to other professionals when they feel there is a need for social intervention. Indeed, this shift away from a biomedical to a more psychosocial approach has seen the development of new roles within Tower Hamlets including social prescribers and care navigators. With 1 in 5 patients visiting their GP with non-medical problems such as employment, immigration, housing and welfare issues, these new roles have a significant part to play in the care landscape and should be at the centre of future system and service development. In Tower Hamlets, GPs have remarked on the crucial role that care navigators and social workers can play as there is growing recognition of issues associated with the wider social determinants of health.
The evidence for the effectiveness of improving patient and health service outcomes for integrated care has been mixed at best. Initially most integrated care programmes were based on case management, which means identifying the top 2-3% of the population (the most complex adults) most at risks of hospital admission. However, now there is increasingly a move towards looking at whole population health needs, with a stronger focus on prevention and management rather than treatment. Whether there is the capacity on the ground to do so, I’m not entirely sure. In fact, based on my emerging findings we are no closer (if not further away) from Andrew Lansley’s somewhat utopian vision of several local fully integrated health and social care systems – it could be argued that care services have actually become more fragmented due to dwindling resources, workforce shortages and low levels of morale among our frontline professionals.
In Tower Hamlets, however, there is growing effort in generating connections and strengthening relationships among different professionals and across different health and social care organisations. Multi-professional teams are an important way of addressing siloed and disjointed working and hence, addressing the differences in professional culture will be integral to enabling partnership working to be effective. This is an important lesson for those embarking on integration programmes – one person’s integration is another person’s fragmentation (Leutz et al, 1999), thus, harmonising the health and social care workforce will be a key facilitator in fostering positive population health outcomes. A bottom-up approach with empowered multi-professional teams focussed on meeting the specific needs of the local population might finally help us deliver what until now has been mainly rhetoric: patient-centred care.
 Close
Close









