Early Career Innovators: Improving Nerve Regeneration with Chemokine Receptor Inhibitors, Repurposing TIN
By Alina Shrourou, on 5 May 2021
In this Repurposing TIN interview as part of the Early Career Innovators series, recognising the amazing translational work being done by postdoc and non-tenured researchers within the UCL Therapeutic Innovation Networks (TINs), Dr Guillem Mòdol Caballero highlights his Repurposing TIN Pilot Data Fund awarded project, involving the use of chemokines as a novel target to improve peripheral nerve regeneration.
What is the title of your project and what does it involve?
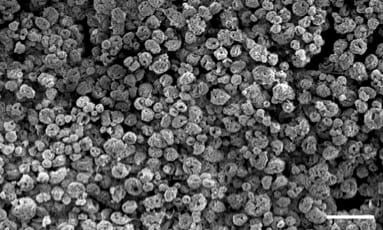
The title of my project is “Chemokines as a novel target to improve peripheral nerve regeneration”. Treatments for nerve injuries have changed little over the last few decades and have significant limitations. The Lloyd lab, of which I am a part of, has previously identified Schwann cells, the major glial cells of the peripheral nervous system (PNS), as orchestrators of peripheral nerve regeneration. Recently, the Lloyd lab has identified a chemokine as a Schwann Cell chemotactic factor, secreted after nerve injury, that is likely to be important in directing the regeneration process. Nerve injuries are frequently associated with aberrant nerve regeneration that can lead to the formation of neuromas and neuropathic pain. Our goal is to determine whether using a chemokine receptor inhibitor, we can limit the Schwann Cell migration that leads to aberrant nerve regeneration and reduce the associated pain response.
What is the motivation behind your project/therapeutic?
The incidence of peripheral nerve injury is estimated to be between 13 and 23 per 100,000 people per year in developed countries. Currently, surgery is the conventional approach to repair nerve injuries but when there is a significant gap between nerve ends, an autologous nerve graft (autograft) is used. Although this is the current gold standard for treatment, autografts present several limitations and engineering strategies such as artificial nerve conduits have not been able to significantly improve the results. The unmet patient need include an often incomplete sensory and motor function recovery, neuroma formation or development of intractable neuropathic pain. Therefore, there is an urgent need to develop alternative approaches to treat peripheral nerve injuries and to prevent maladaptive regeneration, such as during tumour formation or neuroma development.
Can you highlight any challenges have you experienced as an early career researcher in the repurposing/translational research space?
I started working in the translational research space during my PhD and I would highlight that a particular challenge is the funding limitation. Even when the therapies results are promising and are likely to be taken to the clinic, this limitation could even slow down the research. Additionally as an early career researcher, another challenge I have faced is finding collaborations with pharmaceutical companies to help develop these therapies.
Why did you want to apply to the Repurposing TIN Pilot Data Fund?
Considering our last findings on the nerve regeneration process, we wanted to take our research towards the clinic. I thought that the Repurposing TIN Pilot Data Fund scheme would be the perfect fit to carry out this project since we wanted to use a marketed drug, and it would allow us to explore its potential as a treatment for nerve injuries associated with aberrant nerve regeneration.
How did you find the process for the TIN Pilot Data Fund? What did you learn?
The process for the TIN Pilot Data Fund was exciting and really fast. First, I attended the ACCELERATE training workshop and it helped me understanding not only what was required for the particular funding schemes but also the translational path. I also learnt how to be more concise with my scientific ideas when writing the application. My proposal was then shortlisted for a pitching event where we had to present our project. We received a brilliant training session that allowed me to learn how to address the pitch and connect with the audience. Overall, it was a great experience that will help me applying for future grant applications, especially for translational awards.
What do you hope to achieve in the 6 months duration of your project?
I hope to elucidate whether the treatment with the chemokine receptor inhibitor has an effect limiting the Schwann Cell migration that leads to aberrant nerve regeneration in our nerve injury model. The results obtained will allow us to improve the understanding of the nerve regeneration process. I hope this study will help us achieve more funding in the future to bring this potential therapy closer to the clinical translation. This could represent a major breakthrough in the peripheral nerve regeneration field due to the current treatment limitations.
About Dr Guillem Mòdol Caballero
Dr Guillem Mòdol Caballero is a neuroscientist that works as a Research Fellow in the Lloyd Lab, at the Laboratory for Molecular Cell Biology (LMCB) at UCL. During his PhD at Universitat Autònoma de Barcelona he evaluated the therapeutic benefits of delivering Neuregulin 1 (NRG1) to the central and the peripheral nervous systems, as a strategy to treat amyotrophic lateral sclerosis (ALS).
After finishing his doctoral studies Dr Mòdol Caballero joined the Lloyd Lab in 2019- experts in PNS biology. He is now focusing on understanding the complex multicellular interactions required for peripheral nerve regeneration and developing therapeutic modalities to take this research towards the clinic.
 Close
Close