World TB Day 2019 blog
By Neil Stoker, on 6 April 2019
Professor Neil Stoker attended two events to mark World TB Day 2019; firstly, a reception at the UK Parliament and secondly, our World TB Day Symposium. Neil shares his reflections here.
The political and the personal
“28th of January. We have to strike a pretty miserable deal with our drug resistant TB patients. Their only, though by no means guaranteed, chance of cure is to take up to eight unpalatable and side effect-prone drugs for at least two years. Often after only a couple of weeks of treatment, patients will develop anticipatory gagging and vomiting just on seeing the tablets, or rashes so itchy they excoriate their arms and legs.
“Pyrazinamide can make their joints so painful, it’s difficult to stand. Clofazimine causes their skin to become discoloured like an overcooked fake tan – so that one remaining neighbour who didn’t already know that that patient had TB will now guess. Cycloserine can precipitate neurological and psychiatric symptoms, including psychosis and suicidal ideation.
“Furthermore, the TB patients have to be supervised while they take their tablets every day. It may take them hours to walk to their observational DOTS corner, and then further hours to physically bring themselves to swallow the fistful of pills.
“I visit the house of a patient; despite my entreaties he says ‘no’, he will not come back to treatment. It made him feel too awful, whilst now he feels fine. I asked his brother, how is he really doing? He tells me he continues to lose weight, he coughs all through the day and brings up cupfuls of blood at a time, and his breathing makes strange whistling noises morning, noon and night. The national doctor comes regularly to change the dressings that now cover the open hole leading from his chest wall to the lung underneath, which continually oozes pus. He is watching his brother die slowly and he knows he himself must surely now be infected.”
Those words came from the field blog of UCL researcher Emily Shaw-Wise while volunteering as a doctor for Médecins Sans Frontières in Uzbekistan back in 2013. She read them a few days ago in the imposing State Rooms in Speaker’s House in the Houses of Parliament in London, at a reception held by the All Party Parliamentary Group on Global Tuberculosis. It was attended by a mixed audience that seemed to include people from the worlds of politics, NGOs, funders, researchers – and a patient treated successfully for multidrug resistant (MDR) TB, who was full of praise for her NHS carers.
 Alistair Burt, Minister of State at the Department for International Development, and the two MP chairs of the group – Virendra Sharma and Nick Herbert – had talked about the importance of political will, and the need for continued lobbying both to push TB up the agenda, and also to increase funding.
Alistair Burt, Minister of State at the Department for International Development, and the two MP chairs of the group – Virendra Sharma and Nick Herbert – had talked about the importance of political will, and the need for continued lobbying both to push TB up the agenda, and also to increase funding.
But Emily’s graphic account brought home the reality of the situation in parts of the world for patients, communities, and those working to treat patients and control the spread of the disease. A few years had passed, but it seemed likely that most of it remained accurate. For me, as someone who had always been involved in laboratory research far away from the real world, and just begun working as part of a team looking for more effective treatment of drug-resistant TB, this cut through the detached language of our Standard Operating Procedures and depersonalised data that we collected, and contrasted with the efficiency of our well-funded treatment programme, and made it personal and messy and shocking.
The politics are essential though. Without politics there is no funding, and as TB is largely a disease of the poor, funds are even harder to come by. Emily continued:
“6th of March. Today I’ve started to try out rolling out TB care in a new district with a population of 64,000. There were no second line drugs, no proper DOTs corners, no infection control, no staff training on introducing drug resistant TB, no capacity to culture sputum for drug sensitivity testing. The radiological provision for the entire district is one portable X-ray machine and a room less sturdy than a shed. I have an inpatient ward brimming with cases and over 300 ‘chronic’ TB patients in the community they cannot cure, because they are infected with drug resistant strains. Staff have been rationing a handful of respiratory masks between themselves, reusing them for months.
“The TB epidemic here is out of control. We have insufficient drugs, insufficient global regard for our cause and the threat that our work will collapse as soon as we try to leave. How on earth am I going to be an optimist about this?”
It was startling to hear this, both because it contrasted so much with our surroundings a gilded, historic and generally polite setting, and also because this description of crisis management is not how it should be in a world where the WHO had been promoting and refining DOTS for decades, and who had announced a Sustainable Development Goal of cutting TB deaths by 90% from 2015 rates, by 2030. Eleven years did not seem very far away, with a disease where a patient might need to be treated for 2 years, and developing and carrying out trials to test drugs or vaccines are inevitably far longer. Working with the organism, Mycobacterium tuberculosis (Mtb), is equally slow; I recalled Jo Colston, a leading TB researcher at the MRC National Institute for Medical Research, just before his untimely death, starting a talk with the sentence: “The last of these meetings was three years ago; that means I’ve done two experiments since then.” I wondered how much bearing this date of 2030 had to reality.
 World TB Day is a marker for awareness, reflection and calls to arms. There have been recent international and national initiatives, and signs of political engagement with the problems of TB: The first United Nations High Level meeting on TB was held in September, and was flanked by two UK parliamentary debates: the first Commons debate on TB in 65 years in June 2018, and a debate in Westminster Hall in the week after this reception (APPG-TB webpage; transcript; video).
World TB Day is a marker for awareness, reflection and calls to arms. There have been recent international and national initiatives, and signs of political engagement with the problems of TB: The first United Nations High Level meeting on TB was held in September, and was flanked by two UK parliamentary debates: the first Commons debate on TB in 65 years in June 2018, and a debate in Westminster Hall in the week after this reception (APPG-TB webpage; transcript; video).
I’d read a lot about the UN meeting referred to above and had earlier asked Alistair Burt if it really made a difference. They really do, he replied, they push items up to the top of national and international agendas – for a while at least – so it’s important to capitalise on this moment.
Politics is an essential part of the equation – it provides money, structures, and co-ordination between countries and organizations, and is required to deal with the fact that no nation or pharmaceutical company can solve this difficult problem alone. Any strategy also needs to transcend the volatility of politics: 7 days later Alistair Burt was minister no more. He’d said with a smile in his talk that it was good to be able to think about something other than Brexit, but Brexit – like a cuckoo in the Westminster nest – had squeezed another fledgling over the precipice.
Missing Voices
Three days later, I attended a World TB Day Symposium, led by TB researchers based at UCL, the London School of Hygiene and Tropical Medicine, and this year’s hosts, The Francis Crick Institute. Started in UCL in 2010, these meetings have been a way of marking World TB Day with talks that allow anyone involved with TB in London to get a broad update on the latest developments.
 There were 300 people booked for all or part of the event, about 60% coming from the UK research community, 20% from NHS and community organizations, and most of the rest coming from a mixture of pharma, NGOs and overseas research. With live streaming, and on this occasion, live interaction with UCSF in the USA, and with the head of the National TB Programme in Hanoi, the audience was larger and more diverse than in the past. We were told that this was the first ever tri-national live TB conference, and that we were the largest TB event of its kind in Western Europe – we could either feel proud of that or, as one droll person remarked, rather depressed.
There were 300 people booked for all or part of the event, about 60% coming from the UK research community, 20% from NHS and community organizations, and most of the rest coming from a mixture of pharma, NGOs and overseas research. With live streaming, and on this occasion, live interaction with UCSF in the USA, and with the head of the National TB Programme in Hanoi, the audience was larger and more diverse than in the past. We were told that this was the first ever tri-national live TB conference, and that we were the largest TB event of its kind in Western Europe – we could either feel proud of that or, as one droll person remarked, rather depressed.
This event was also marked by the publication of two TB special issues, by The Lancet, and the International Journal of Infectious Diseases. The WHO 2030 goal was mentioned with some scepticism, by speakers, some of whom were authors in The Lancet issue. One of these, Eric Goosby, Professor of Medicine at UCSF and also UN Special Envoy on Tuberculosis, speaking on video from San Francisco said that at the current rate of decline, the 90% reduction in mortality would not be achieved in a decade, but would actually take over a century.
Here are some comments that struck me during the day (without any attempt to be balanced or comprehensive):
Vaccine hope: There have been some possibly game-changing developments. Rob Wilkinson from The Crick, Imperial College and elsewhere described the first vaccine trial to show preliminary but promising results against active TB disease in South Africa just two months ago. The history of vaccines better than BCG (which is not useful in most global settings today) has been a litany of disappointment, and my expectations had all but disappeared, so these positive results were potentially big news.
Unrealistic targets?: Nim Araniminpathy from Imperial College used mathematical modelling to look for gaps in the care cascade used in TB, and showed that even with what he called UBI models (‘Unrealistically [optimistic] But Informative’), we could not achieve WHO’s goals simply using cure; prevention (for example with a so-far non-existent vaccine) would also be required. He also noted that prevention also included non-medical factors such as nutrition and hygiene (more on social issues below).
The rise of XDR TB: It was quite sobering how quickly XDR (extensively drug-resistant) strains of Mycobacterium tuberculosis (Mtb) have become normalised in talks. Once whispered to hushed audiences as 1 or 2 were identified, they are now ubiquitous.
The need for basic microbiology: Claudio Köser from Cambridge surprised me in saying that some very basic and important information is not present. He discussed the need for practical and careful microbiology, saying that there is not good experimental evidence for some of the doses of TB drugs used. Quality Control in TB has been neglected systematically, he said polemically, but addressing these issues could improve both efficacy and patient experience. There has always been a lot of dogma in TB, so it was good to see this being questioned systematically, although disturbing that it hadn’t been done before.
Biomarker promise: Biomarkers (indirect measures, for example from the blood) that indicate disease earlier than existing tools are very fashionable, but are hard to move into practice. Myrsini Kaforou (Imperial College) showed how they might usefully dissect disease classification, as happens with cancer; Rishi Gupta (UCL) showed that we might be able to identify people for whom preclinical disease is beginning, perhaps 6 months before clinical signs appear. That would provide a much better window for treating disease and preventing transmission.
Tackling social issues: Delia Boccia from LSHTM took a different tack, talking about Social Protection (policies and programs designed to reduce poverty and vulnerability). TB is a disease of poverty, and she presented evidence that increasing spend on this as opposed to treatment could have a substantial impact on TB mortality. She described work in Brazil to help bring people out of poverty, including cash transfers. Such a short conference could not be comprehensive, but it seemed important to include a sociological perspective.
AMR and TB: Dame Sally Davies, currently our Chief Medical Officer, though not for much longer, brought us back to the problem of complexity through Antimicrobial Resistance (AMR), a topic that she has persisted in pushing during her incumbency. AMR can overwhelm us through its complexity, size and intersectionality, she said. It seems to me that TB is not so different, and of course they are each part of the other’s intersectionality. She mixed terrifying numbers with the need for political advocacy.
US perspective: The political slant was echoed by Richard Pan, a scientist turned Californian state senator. He’d stood for office because it seemed wrong to complain about politicians if you weren’t prepared to do something oneself – and he hadn’t expected to be elected. ‘I don’t think people really believe in infectious diseases any more’, he said, adding a new layer of difficulty to the problem. However his solution is clear: ‘We need data, a social strategy, and political will’.
Digital X-rays: The meeting ended with a transatlantic debate. The UK side was led by Liz Corbett, who has worked on TB control for many years in Malawi, currently the fourth poorest country in the world. I was interested that she mentioned that she was feeling positive for the first time in a while about TB control. I asked her why – a mixture of things all coming together, she said – and then added ‘Digital X-rays! They’re brilliant!’. I thought it good to hear that amongst all the talk of molecules, X-rays – those classic diagnosers of TB – still had their place, and technical improvements were changing TB control in a resource-poor environment
Reactions from attendees
A colleague of mine, Julio Ortiz Canseco, whose expertise is microbiology and molecular biology, found the mixing of disciplines refreshing: “The most exciting part of World TB Day is to get the fresh air that provides people looking at the problem with a completely different point of view, such as the economic or the patient sides of things, the politics or the public engagement, rather than the lab version of the problem.”
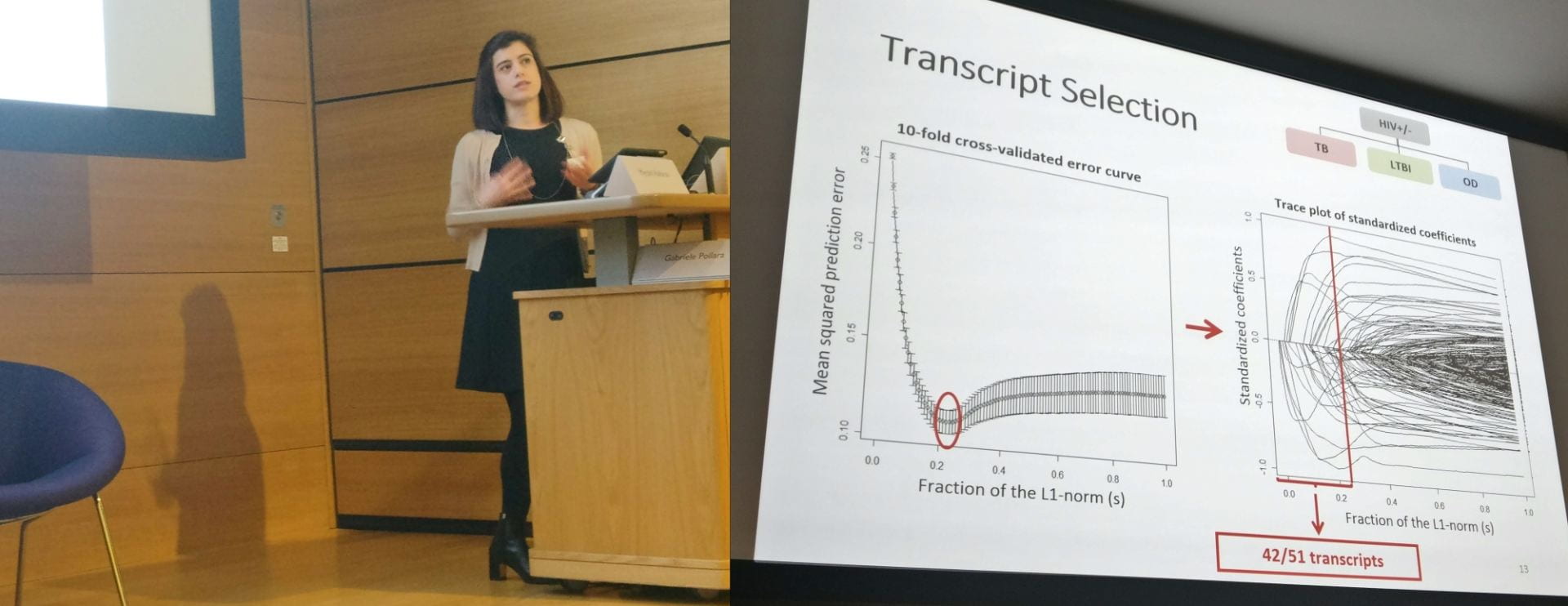
During the day I’d been trying to find out who was attending the meeting apart from the research world I knew well. I talked to a TB nurse, Opal from Newham and St Mary’s Hospital, as she recharged her phone. I asked if the talks were pitched at too expert a level. Many speakers had included slides that I felt took no prisoners (as in the example shown above).
No, they were fine, she said, and I reflected later that maybe I was wrong in thinking all slides should be ‘accessible’. Maybe it’s also useful in this event that tried to bring people from different aspects of TB control together, to step into realities of other people’s worlds, and see what they deal with in all its messy detail. Maybe that helped connect people to what others were doing through awareness that hadn’t been filtered into bland generalisations, just as hearing the details of Emily’s Uzbekistan experience was what was compelling. I also wondered if hearing that detail empowers people to develop of interactional expertise, allowing them to start to be able to communicate with people from different disciplines despite a lack of formal training.
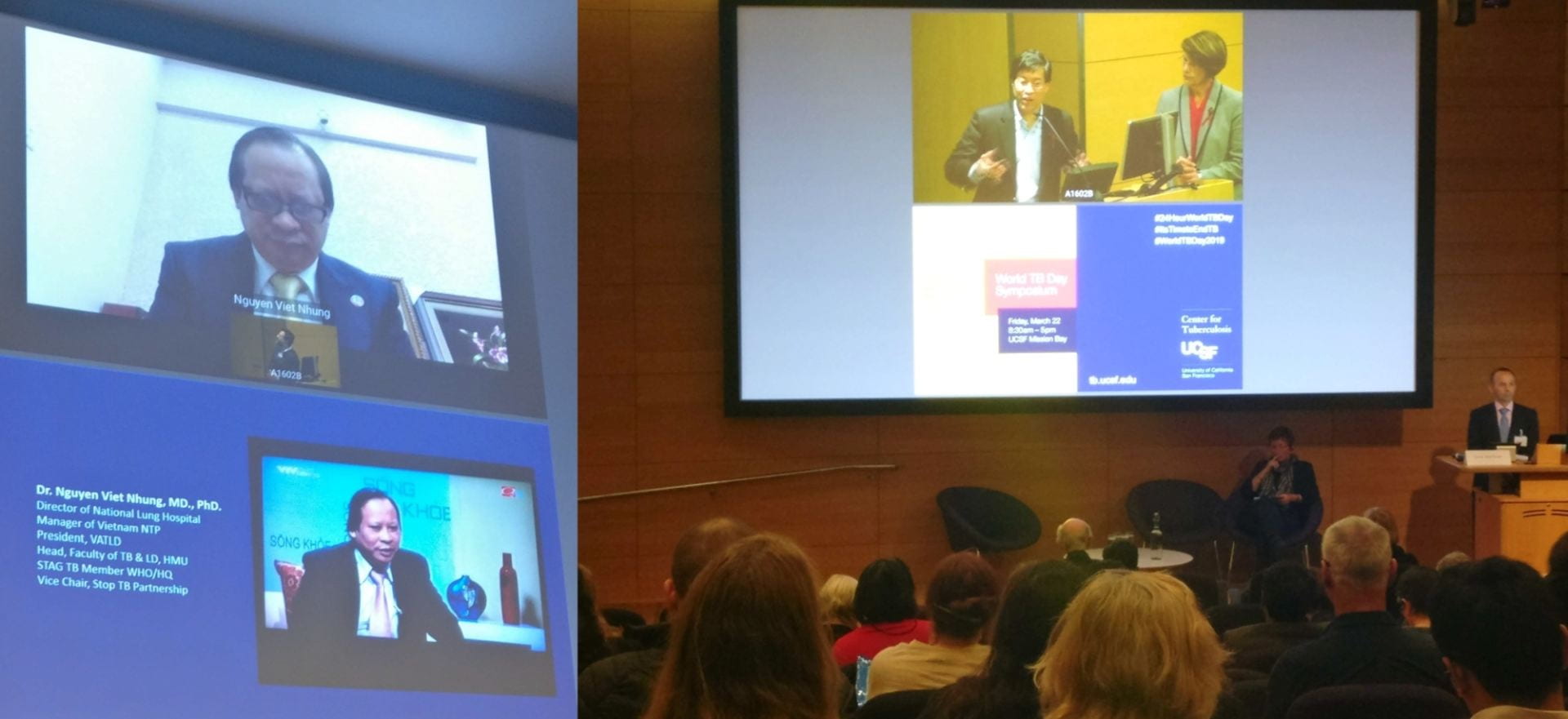
Left: Dr Nguyen Viet Nhung speaking from Hanoi; Right: Senator Richard Pan and Dr Karen Smith, Director of the California Department of Public Health, speaking from San Francisco
The talk that had been most interesting to Opal was that by Delia Boccia, mentioned above. We are trying to overmedicalise something that is a social issue, she said. Treat the poverty, and the TB will go. She’d worked on Hepatitis C, and thought treatment had moved much faster than in TB because – as with HIV – of patient advocacy in rich countries. ‘We leapfrogged you guys!’ she said.
And I was drawn back to Emily’s description of being overwhelmed by patients with TB with almost no equipment or drugs. She was telling us of a patient who was clearly dying.
“She’s in acute respiratory distress syndrome, and is effectively drowning. I bark a shopping list of drugs and equipment at a nurse, she looks at me blankly and then returns with one 500ml bag of fluid”.
She concluded:
“Every death from TB is avoidable, Forget the technical details about tissue necrosis [and so on]. All deaths in TB boil down to lack of commitment from the International community. I cannot draw any comfort from [this woman’s] death, but maybe her story will spur you on to take additional steps to join in the fight against TB.”
I thought about how unusual it had been for me to have heard Emily’s personal experience, and how important her perspective was. She had spoken for the 10 million people who develop TB disease every year, and the 1.6 million who die, for the many more whose lives are affected indirectly by the disease, who are effectively silent in this discourse. I wondered how different things would be if these people were able to speak, and demand more resources, research, and involvement. Would our research look different? And would that pressure already have led to more effective, less toxic, treatments, and effective prevention?
Neil (ORCID ID) is a Clinical Trials Quality Assurance and Data Manager in the Centre for Clinical Microbiology at UCL, working on TB Alliance-funded phase 3 trials Zenix and SimpliciTB to improve treatment of MDR and XDR TB. (The views expressed in this blog above are his personal views and not those of any of the organisations mentioned here.)
Read more of Emily’s blogs about working with MSF in Uzbekistan here.
 Close
Close