IoMH Conference 2023 – a PhD student’s report
By iomh, on 29 September 2023
The fourth UCL Institute of Mental Health Conference explored a diverse range of topics including health economics, suicide prevention and cognitive neuroscience. UCL Wellcome PhD student Jennifer Fielder shares some of her highlights of the day.

As a PhD student in Mental Health Science, I was excited to hear some of the latest mental health research showcased by leading experts at the Institute of Mental Health (IoMH) Conference.
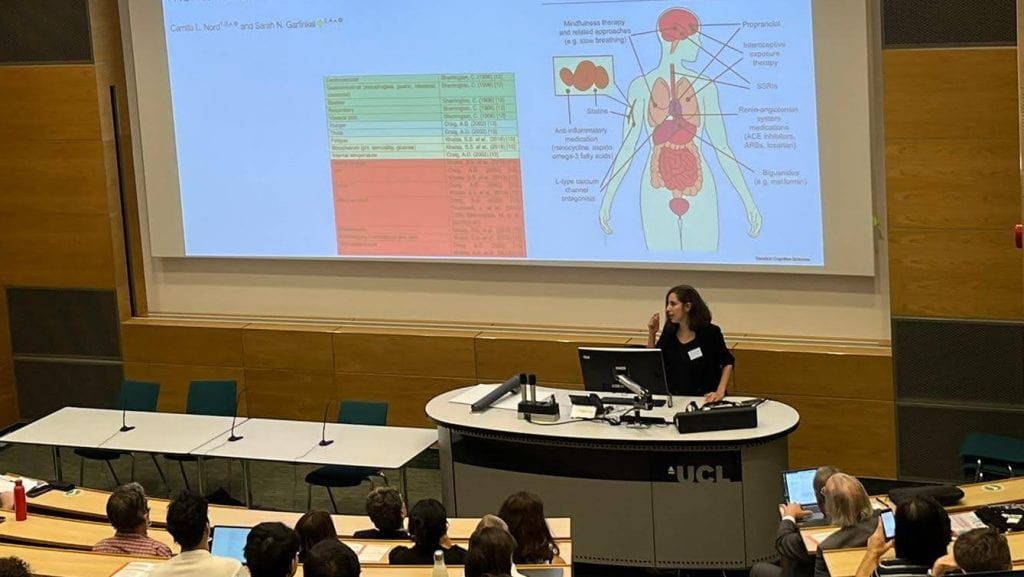
The first session on mind and body interactions followed warm welcomes from Professor Anthony David, director of UCL IoMH, and Professor Alan Thompson, Dean of the UCL Faculty of Brain Sciences. UCL’s Professor Sarah Garfinkel focused on how our ability to sense internal contexts and signals, known as interoception, shapes mental health. This covered her work on interoceptive training, where people learn to detect their heartbeats more accurately, which decreased anxiety in autistic adults for up to one year after the training. The talk finished with the exciting prospect that effective psychiatric treatments may work via interoceptive pathways. For example, one dose of the antidepressant Citalopram was found to increase interoceptive accuracy.
Having highlighted the importance of mind-body interactions in mental health, the stage was set for Professor Carmine Pariante from King’s College London to present his research on the immune system and depression. Professor Pariante presented evidence from large datasets, such as UK Biobank and the BIODEP study, showing the association between high levels of inflammation (C-reactive protein markers) with treatment-resistant depression even when controlling for confounders. This highlighted potential for a clinical trial using anti-inflammatory treatments for those with few options for depression treatment.
The next session, “How to fund a National (mental) Health Service” kicked off with Professor Martin Knapp from the Department of Health Policy at London School of Economics and Political Science (LSE) who presented evidence that despite increases to funding and workforce the NHS was not keeping up with demand. Mental health accounts for 23% of the UK’s burden of disease, yet receives only 13% of NHS funding. Professor Knapp presented estimates from the LSE-Lancet Commission on the Future of the NHS that general taxation would only need to increase by 1 or 2p to generate sufficient funding, making it clear that a small investment could make the world of difference. Is a high-performing mental health sector really out of reach?
Economic arguments
Dr Lade Smith CBE, President of the Royal College of Psychiatrists, provided some contextual facts of the mental health sector and argued that as well as knowing how to fund it, politicians need their why. That ‘why’ from many of the audience members would perhaps be fairness and relieving suffering, however the political and economic argument is in productivity and prosperity, explained Dr Smith. Unlike physical health, 75% of mental health conditions start before the age of 25. These young people haven’t reached their peak productivity and inadequately preventing and addressing mental ill health will hinder economic and educational potential. Dr Smith pointed out that 1.3 million people are economically inactive in the UK, and mental health problems are now a greater barrier to employment than musculoskeletal problems. Dr Smith argued that if politicians want an economically productive society, investing in mental health is key.

The final discussant of the session was Professor Tim Kendall, NHS England’s National Clinical Director for Mental Health who immediately acknowledged the underfunding of the NHS, but highlighted improvements such as the investment into school-based mental health teams. Professor Kendall echoed points made by Professor Knapp and Dr Smith, that the future hinges on prevention, early intervention and focusing on inequalities. Anti-bullying measures in schools to prevent future mental health problems and collaboration to address multiple determinants of mental health were discussed, further emphasising the “whole-of-society” responsibility – not just the NHS.
‘Societal values’
The third session was a juxtaposition of two talks about suicide and mental health: suicide prevention and assisted suicide. Professor Sir Louis Appleby from the University of Manchester and government advisor on suicide prevention, discussed the recently released National Suicide Prevention Strategy. The talk highlighted the most at-risk group being middle-aged men, and of those who died by suicide, characteristics such as economic instability, alcohol use and (often untreated) mental health problems were most common. However, it is too simplistic to say that middle-aged men are not seeking support. Two thirds had contacted services within the three months prior to death, with a third making contact the week prior. Other priority groups are those in mental health care and young people. Each group have different risks and needs, as emphasised in ethnic minority groups, and the new strategy has had to recognise this. Professor Appleby ended the talk in reference to sociologist Emile Durkheim with the question of: “What kind of societal values do we want to live by to maximise fulfilment?” We all have a role to play in suicide prevention.

The next session about psychiatric euthanasia and/or assisted suicide (EAS) was by Dr Scott Kim from the Department of Bioethics at the National Institutes of Health, USA. The talk focused on data from countries where it is legal, including The Netherlands, Canada and Belgium. Dr Kim presented evidence on EAS requests, around 70% of which are from women. Dr Kim concluded that among depressed patients ill enough to be eligible for EAS, most usually get better, and we cannot accurately predict who will. The important implication of these findings is that psychiatric EAS for depression will result in many who die unnecessarily and prematurely.
The final session by Professor Sophie Scott, Director of UCL Institute of Cognitive Neuroscience, was about laughter. The physiological effects of laughter include a reduction in adrenaline, reduction of cortisol and increased uptake of endorphins. Professor Scott discussed how laughter could be used as a tool to examine social relationships which may be useful for mental health science.

Alongside all the talks were brilliant posters of current research in mental health science. Congratulations to poster winners Sarah Buehler, Merle Schlief, Laura Grover and Davin Schmidt.
Thank you to all the speakers and the audience for asking great questions, and to the IoMH for organising the event to bring all those interested in mental health research, practice and policy altogether.
This blog includes contributions and edits by Humma Andleeb. You can read Humma’s thread about the event on Twitter/X
And more tweets from the conference can be found through the #IoMHconf2023 hashtag.
To hear more from Professor Sir Louis Appleby and Dr Scott Kim, you can find podcasts by with IoMH PhD students on the Mental Elf YouTube Channel.
 Close
Close

