Early Career Innovators: Cell Replacement Therapy in Alzheimer’s Disease, Regenerative Medicine TIN
By Alina Shrourou, on 11 August 2021
In this Regenerative Medicine TIN interview as part of the Early Career Innovators series, recognising the amazing translational work being done by postdoc and non-tenured researchers within the UCL Therapeutic Innovation Networks (TINs), Dr Charlie Arber highlights his Regenerative Medicine TIN Pilot Data Fund awarded project, involving the potential of stem cells in Alzheimer’s.
What is the title of your project and what does it involve?
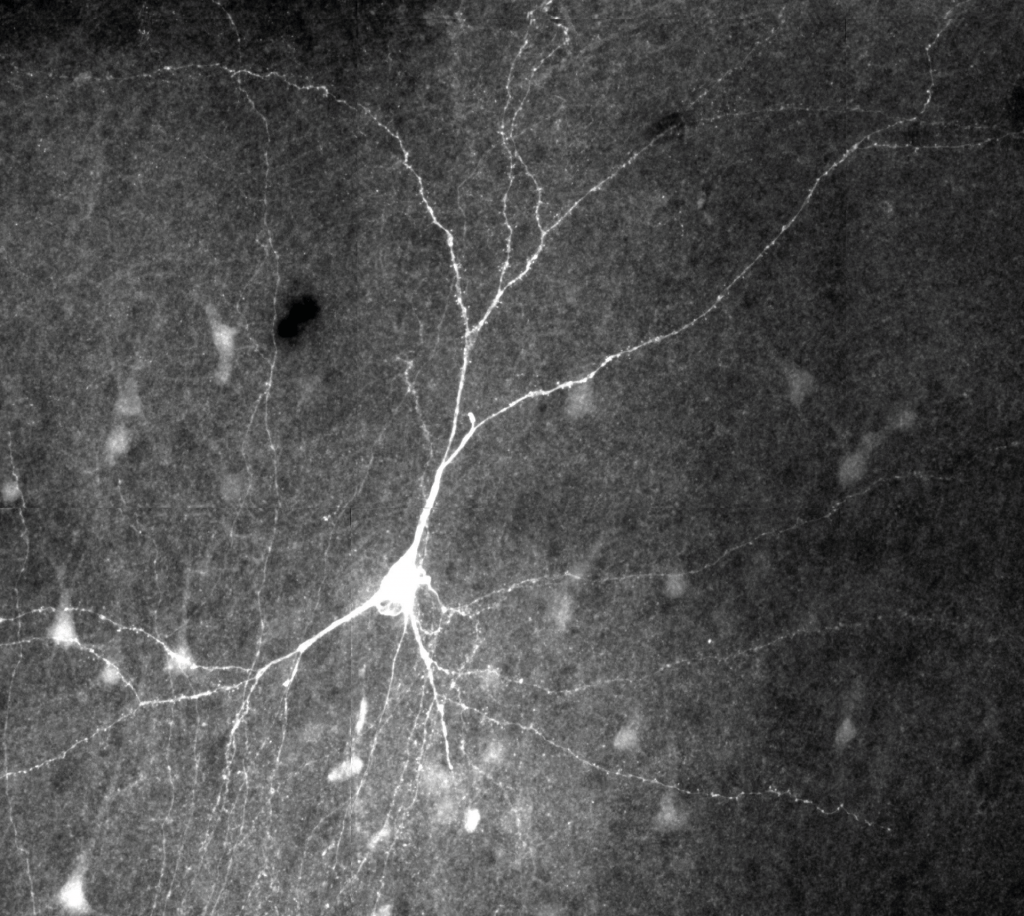
The Regenerative Medicine TIN have supported my project titled “Cell therapy in Alzheimer’s disease”. This is a project to understand the potential of stem cell derived astrocytes in repairing the brain in the dementia. Astrocytes are brain support cells, capable of cleaning the brain and even replacing some of the cells that degenerate in disease.
The project will answer three questions:
- Can human astrocytes interact with mouse brain slice cultures?
- Can astrocytes change the inflammatory state of the brain?
- Can astrocytes sense and respond to amyloid (the main pathology in Alzheimer’s disease)?
What is the motivation behind your project/therapeutic?
There remain no therapies to slow, reverse or prevent dementia. In 100 years, how will we treat dementia? Possibly by replacing the cells that have degenerated? Like Luke Skywalker’s hand? This project is a first step to understand the value of astrocytes in cell replacement therapy in Alzheimer’s disease.
Can you highlight any challenges have you experienced as an early career researcher in the regenerative medicine/translational research space?
I am a basic scientist. I think understanding the importance of basic biology in translational science is under-appreciated. All basic scientists should have translational goals. This is the major impact of our work.
I have found keeping an eye on the larger picture and the long term goals a challenging aspect to my career. Small pilot grants such as the initiatives from the TINs have an invaluable role in supporting this type of research.
Why did you want to apply to the Regenerative Medicine TIN Pilot Data Fund?
It is often hard to generate the pilot data that is required to apply for large grants and fellowships. I applied to the Regenerative Medicine TIN Pilot Data Scheme to learn a new technique (organotypic slice culturing) that has enabled me to generate new data which will be central to my fellowship applications and my career progression.
Join the Regenerative Medicine TIN to be the first to hear about similar opportunities
How did you find the process for the TIN Pilot Data Fund? What did you learn?
I found the application process straight forward. Before the dragon’s den style interview, we had interview/pitch training from a professional coach, provided through ACCELERATE. I received some really useful feedback, especially in conveying a message in just two slides and 5 minutes.
Learn more about the training offered through ACCELERATE Success
Since the project began, I have had useful experience in budgeting for a small grant and deadline management due to the short, 6 month nature of these projects (as well as COVID-related setbacks!).
What do you hope to achieve in the 6 months duration of your project?
Having had this opportunity and support from the Regenerative Medicine TIN, I have generated some interesting and exciting pilot data. I am now looking forward to building on these findings as a major thread of my research career. I really look forward to driving this research question forward.
About Dr Charlie Arber
Charlie Arber is a stem cell biologist. He has worked with human stem cells for 15 years, understanding the best ways to make brain cells in a dish and using stem cells from patients to investigate the earliest causes of dementia.
Charlie is a senior research fellow in the department of neurodegenerative disease at the Institute of Neurology. His current research focus is looking at the role of brain inflammation in early onset Alzheimer’s disease.
 Close
Close