Getting inspired: Community Navigator Study Working Group Meeting 2
By Kate C Fullarton, on 6 June 2016
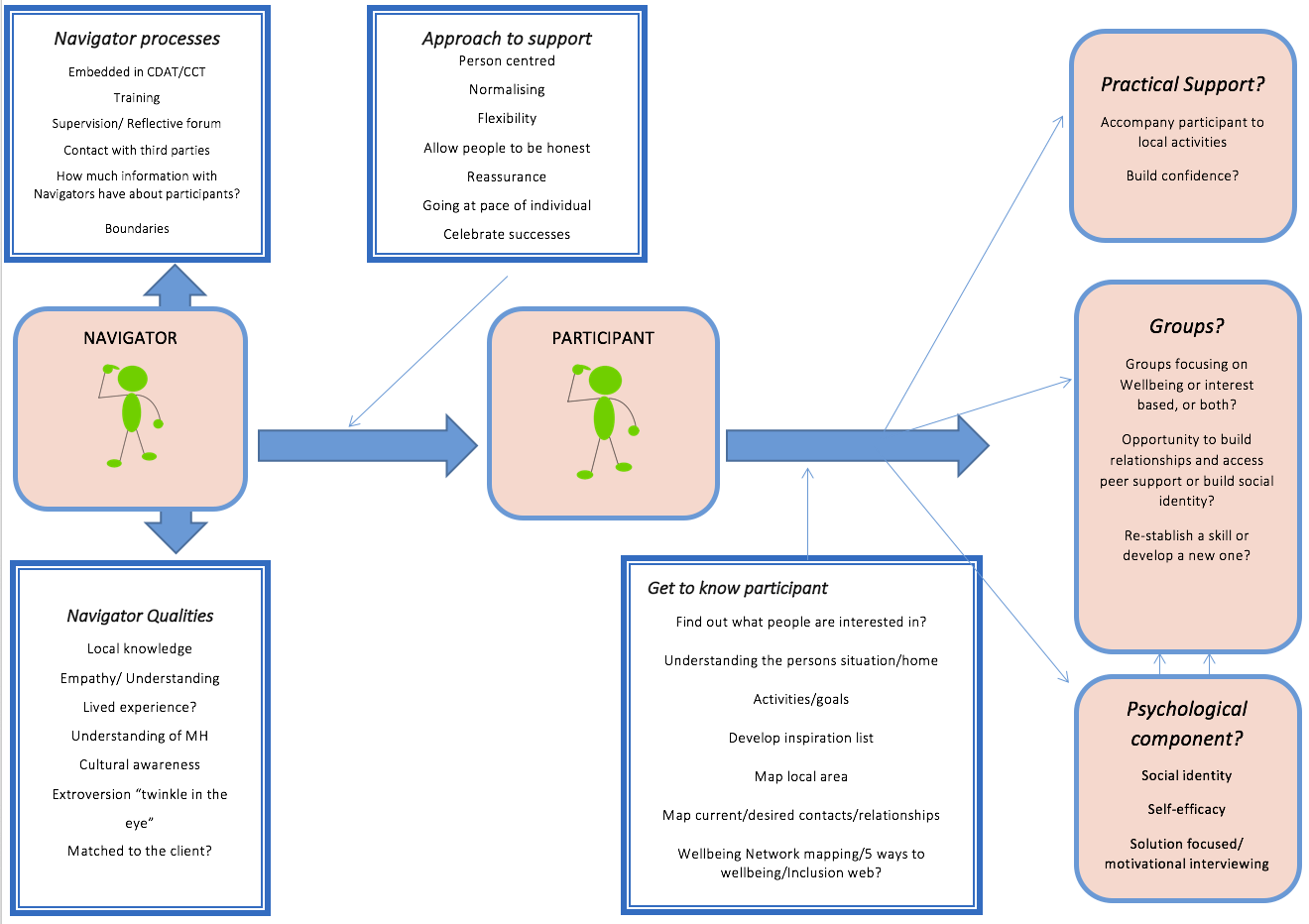
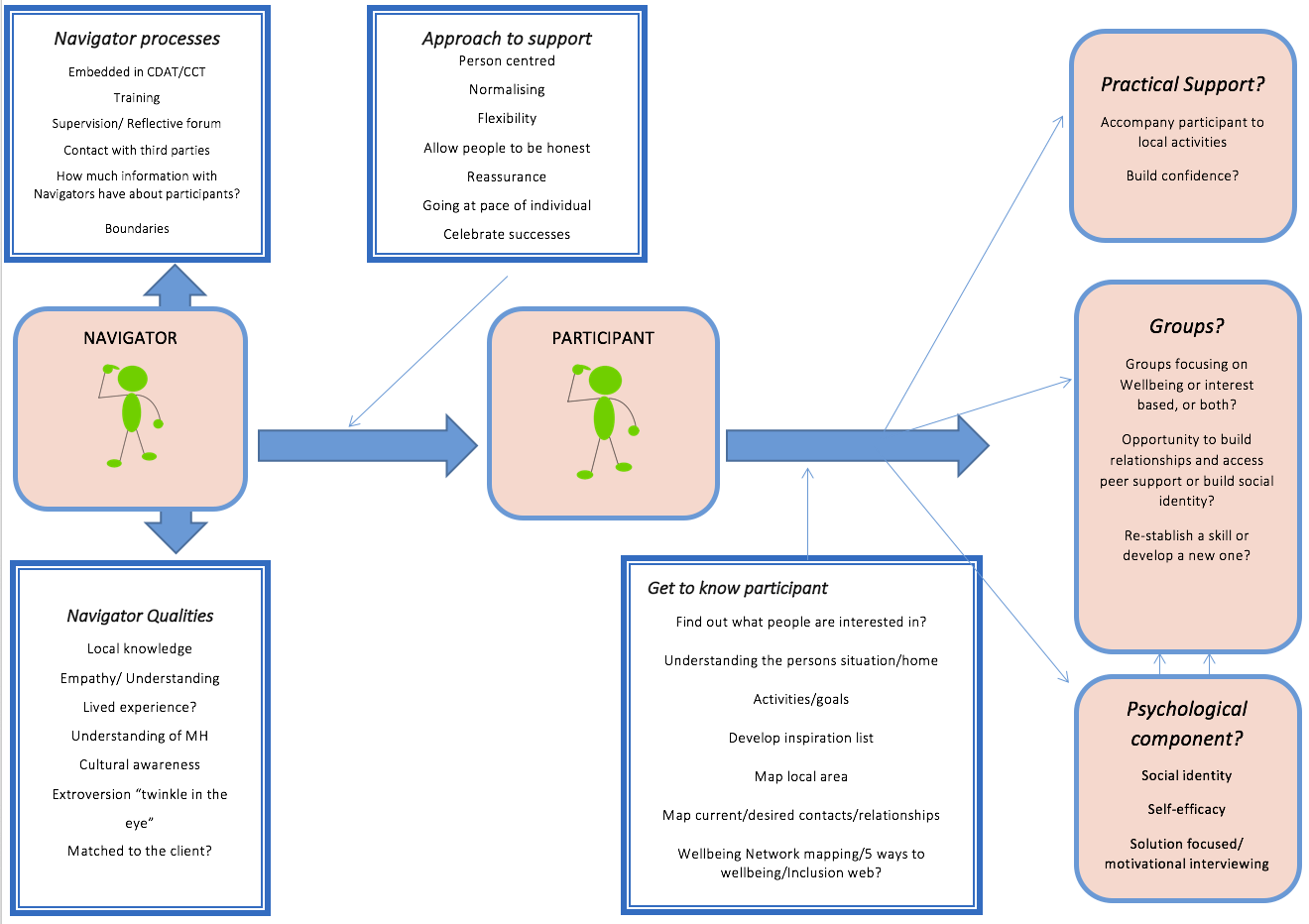
We kicked off our second working group meeting by reflecting on the model that we began building in our first session. It was a useful reminder of how much was achieved in just a single meeting, and provided a framework on which to build.
Model from Week 1
We then heard from Helen McPeake, a Senior Project Manager from Wellbeing Enterprises (WE), an organisation based in Merseyside, which works to improve the health and wellbeing of local communities, by tackling loneliness and isolation. The interest and engagement in WE’s work was clear, prompting questions from around the room. Helen answered all of our questions and we gained a very clear sense of the WE model.
WE have Community Wellbeing Officers based in GP practices who work with people to empower them to ‘talk’, ‘connect’ and ‘take action’. The wellbeing officers focus solely on social issues, helping service users improve social support and access groups and services. This process begins with a ‘wellbeing review’, which lasts around forty minutes and allows people to talk about what is bothering them and what they might like to be doing more of in their lives. The Wellbeing Officer then works with the person to set goals around connecting with practical support, services, activities and other people in the community. The Wellbeing Officer may also refer people to ‘Social Prescribing Programmes’ which are short courses available through WE. After three, nine and twelve months, the Wellbeing Officers meet again with people or arrange telephone follow-ups.
Learning more about WE and the impact they have had in their community was inspiring for us all. One of the big questions we had for Helen was how she saw this working for people who are using secondary mental health services for persistent anxiety or depression and perhaps have more complex needs. What was particularly inspiring was hearing Helen describe the WE ethos as truly person-centred and the ‘can do’ attitude of WE practitioners, consistently reassuring us that it doesn’t matter about a person’s diagnosis or their past, but about what can be done now. A phrase that kept coming up was ‘What is the most important goal for you right now?’
As she spoke, a palpable feeling of optimism grew around the room, and after a short break, we began to capitalise on all the ideas that her talk had sparked. We divided ourselves into pairs and on a copy of the model from the first meeting, added, changed or removed anything from the model as we felt was needed, before discussing these ideas as a group.
Comparing our work from the first and second meetings, it’s exciting to see how our model is developing as new ideas are added. We’re also coming up with lots of questions about what exactly the community navigator support should look like, which we’ll definitely be returning to.
Model from Week 2
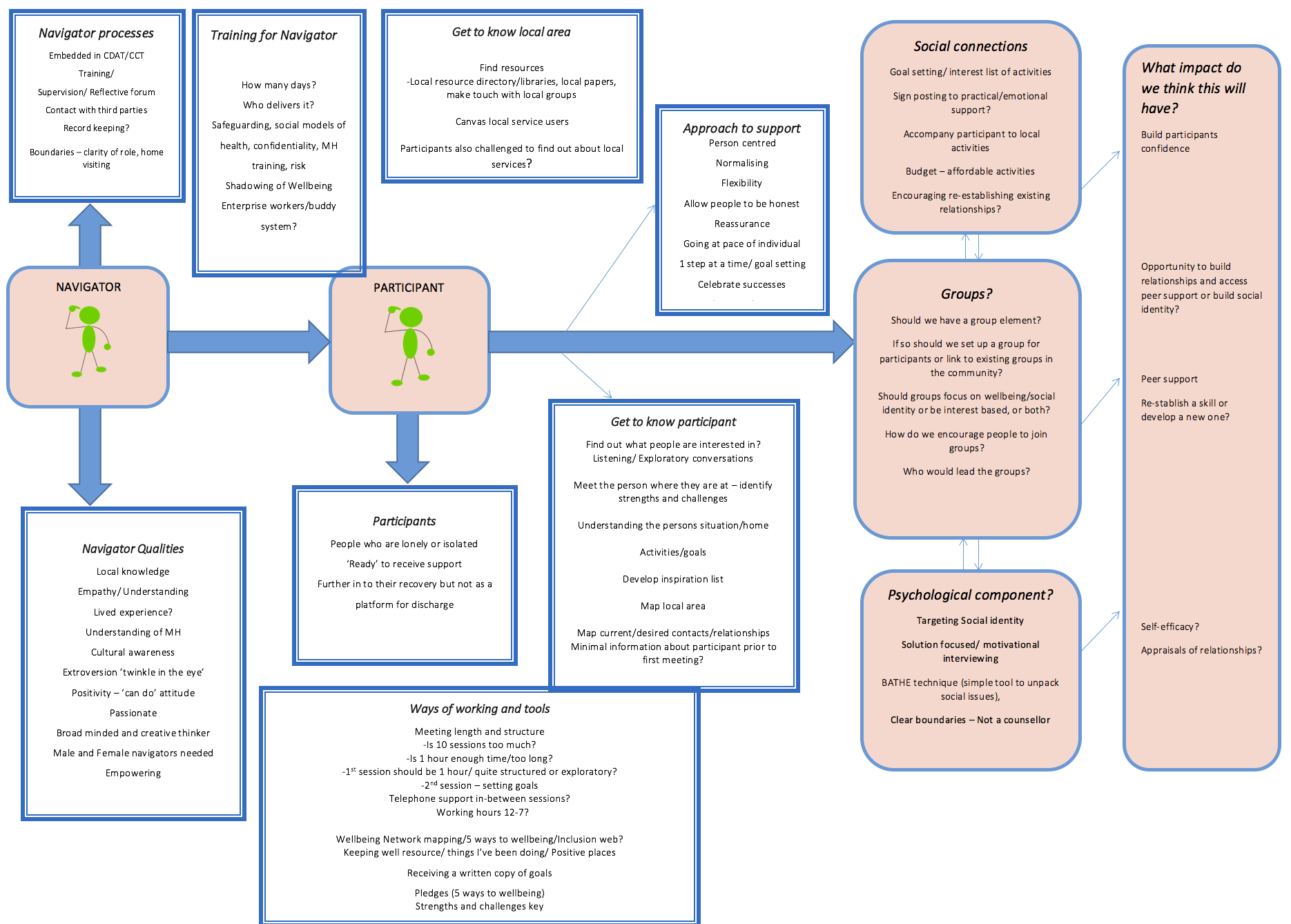
Some of these questions include: should we be connecting participants to pre-existing groups in the community or should we be setting up our own groups for participants to attend like Wellbeing Enterprises have? If so, should these be well-being focused groups, such as mindfulness, or should they be more activity based and interest-led? The various benefits and drawbacks of these approaches were discussed, and we’ll come back to these ideas in future weeks as we begin to make decisions about the programme of support. Another question that came up was the length and structure of sessions over the six months that participants receive support from a community navigator. Helen explained how much could be achieved in relatively fewer and briefer sessions, when they are clearly structured, but would this work for people with complex needs? What are your thoughts? Is 10 sessions over a 6 month period too much? Or perhaps it’s about right, or not long enough?
We’ve also created a new column, on the right hand side of the model, headed ‘What impact do we think this will have?’ This is to make sure we that when we make decisions about what the community navigator support includes, we are basing this on a clear rationale about why we think that element will reduce feelings of loneliness.
Bringing us back to reality a bit, we then heard from one of the practitioners on our working group, who discussed the current challenges to delivering this type of support within a secondary mental health service setting, reminding us of the context the Community Navigators will be working in. There does seem to be real enthusiasm for the Community Navigator role amongst the participating services, however, and a strong sense that this type of support should be beneficial to service users, so the atmosphere of optimism was not diminished.
As this meeting was nearing its end, we then turned to Bryn, one of the co-leads on the study to discuss the Community Navigator job advert. This is now live, so if you’re interested, take a look, and apply here.
We’ll next be blogging after our meeting on 31st May, when we’ll hear from Peter Bates, who will be visiting to talk about his work alongside the National Development Team for Inclusion.
Until then we would love to hear your thoughts on our key questions. These include:
Should the support include a group aspect? If so, what type of group? Should we be targeting the psychological aspects of loneliness or focusing on helping increase social activities?
Get in touch with your thoughts on Twitter or get in touch with Kate, the UCL researcher, by emailing k.fullarton@ucl.ac.uk.
If you want to know more about the study, please view our main webpage.
Getting started: Community Navigator Study Working Group Meeting 1
By Kate C Fullarton, on 26 May 2016
On 26th April, a group of researchers from UCL and the McPin Foundation, people with lived experience of mental health problems and staff from the Complex Depression, Anxiety and Trauma (CDAT) service at Camden and Islington NHS Foundation Trust and the Complex Care Team (CCT) at Barnet, Enfield and Haringey NHS Mental Health Trust, came together for the study’s first working group. What is so exciting about this project, is being able to bring together people with such varied experiences, perspectives and expertise, to work out what the community navigator support should look like: What skills, qualities and experience should our community navigators have? How can they best support people to make social connections and access activities in their community? These are just some of the questions that we’ll try and come up with an answer to over the course of the project, and particularly in the next few months.
We began the session by looking at the initial plans for the study (click to see the presentation slides), before discussing the principles of co-production and how we could use these principles to inform how we work together as a group (click to read more about the co-production approach that we’re using in the study). We later had a whistle-stop tour through theories of loneliness and some existing projects such as Wellbeing Enterprises, Groups4health and Connecting People Study which helped us to begin thinking about the core elements of our model: what are we trying to target when we talk about loneliness? What methods do these existing projects use to help people feel less lonely? What tools can we use to begin talking with people about their social world? The most striking thing about this presentation, which can be accessed here , was the lack of research evidence outlining effective methods for reducing loneliness among people with mental health problems. This gives purpose to why we are doing this project and serves as a powerful motivator for designing the best possible model of support that we can.
A particularly productive conversation resulted from everyone in the room splitting off into their primary group of expertise: practitioner, expert through lived experience or researcher. Each group was given a piece of flip chart paper and asked to put down their ideas for the community navigator support. We then came back together and discussed our ideas. These focused on the content of the support, the role of the community navigators and key questions which we’ll need to address before the community navigators’ work begins. What was interesting was that each of the groups came at this task from slightly different angles, reflecting their different perspectives of mental health services and providing a clear demonstration of how beneficial the co-production model will be.
This model illustrates the initial ideas the group had about the role of the community navigators and the support they will provide. What do you think? Is there anything that we’ve missed that should be added?
Despite really useful and animated discussions about community navigator support and the project more generally, we had run out of time and had to bring the first meeting to a close. Here, we’ve captured some reflections from people who attended:
“Healthy relationships are key to everyone’s mental wellbeing. Sometimes, traditional mental health ‘treatments’ don’t allow time to explore and address the other factors that are making a person feel isolated and lonely. Our communities often have rich untapped resources but that require some support to navigate. It is exciting to be involved in a project that is specifically working towards helping people to build social connections in a way that is meaningful to them.”
“I hope that our project will enable people like myself to begin to take their first steps forwards. For three years I struggled with agoraphobia, feeling frightened, alone and depressed, completely trapped in my isolation. One of my many hopes for our project is that we help more people like me to know that they are not alone.”
Another member of the group, working at Barnet, Enfield and Haringey (BEH) Mental Health Trust, said:
“At BEH we are delighted to be involved in this research project. Often loneliness is an issue under the radar of services despite the impact it can have on service users’ quality of life.”
We’ll be blogging again after our next meetings on 10th and 31st May. On 10th, we’re looking forward to hearing from Helen McPeake from Wellbeing Enterprises about the inspiring work they are doing in Merseyside and on 31st, Peter Bates , will be visiting to talk about his work developing training resources for staff in the National Development Team for Inclusion.
We’ll also be coming back to our model each week and seeing how what we’ve learnt can develop the model further.
If you want to know more about the study, please view our main webpage and check out the McPin blog.
Do you have any thoughts about the role of community navigators? Get in touch with Kate, the UCL researcher, by emailing k.fullarton@ucl.ac.uk.
LonDownS makes local news in Berkshire
By rejutal, on 14 April 2016
The LonDownS study, looking at dementia in people with Down syndrome and led by André Strydom, has made the local press in Berkshire.
Berkshire Healthcare NHS Trust is taking part in the LonDownS study for over a year now and has recruited and assessed several people using the LonDownS battery of assessments.
See the full press release here: https://t.co/grjC5LyzLd

New MSNAP Standards recognise importance of age appropriate care for Young Onset Dementia
By rejujec, on 8 April 2016
A submission by Dr Janet Carter to the Memory Service National Accreditation Programme (MSNAP), run by the Royal College of Psychiatrists, has led to the adoption of new national standards for Young Onset Dementia (YOD). The role of MSNAP is to help improve the quality of memory services in the UK and to set national standards for those running memory services whether or not they belong to the programme.
Dr Carter is member of the National Young Onset Dementia Network, hosted by the charity Youngdementia UK which is committed to improving care for younger people and their families living with dementia. For the first time, standards designating a clear care pathway and a named lead for YOD have been identified. The submission was supported by evidence from the UK survey of services for YOD published earlier this year by Dr Jo Rodda and Dr Carter.
Community Navigator Study: Mental health service users wanted to join our working group
By Jake Fairnie, on 31 March 2016
Our new research study is looking for up to 5 people with personal experience of mental health problems to advise on developing and testing a programme of support for mental health service users which aims to increase people’s community connections and reduce loneliness.
Loneliness can affect people in all walks of life. A recent UK survey found that 28% of people wish they have more friends. Most public programmes, such as the Campaign to End Loneliness1, and most research on loneliness, has focused on older people. But there is growing evidence that loneliness has a range of harmful effects on health and quality of life for people of all ages. People with mental health problems report having less contact with family and friends than people in the general population do, and are particularly vulnerable to loneliness. Being lonely increases your chances of becoming depressed, and for people with mental health problems like depression and anxiety, also being lonely reduces your chances of a speedy recovery.
So finding ways to help people develop community connections may be a big help to improving people’s quality of life, and lead to a range of physical and mental health benefits. But this type of help is often not provided in mental health services, where staff time is limited and the focus can be more on medical or psychological treatments. There are a number of innovative projects happening across the country which may help people develop more connections. Community navigation projects help people review activities and places they enjoy, and people they like seeing, then support people in re-establishing social contacts or trying new things and meeting new people. But we lack good research evidence about how effective these projects are or how they may work best for people with different mental health conditions.
A research team from University College London and the McPin Foundation has secured funding from the School for Social Care Research (part of the National Institute for Health Research) for a Community Navigators research study. The study is led by Professor Sonia Johnson and Dr Brynmor Lloyd-Evans at UCL, and will work with mental health services in Camden, Islington and Barnet. Over a 2-year study, we will develop and test a programme of support for people with anxiety or depression using specialist mental health services, to help them increase their community connections and social contact, with the aim of helping to reduce loneliness. The support will be provided by paid Community Navigators. We will work to develop our programme with organisations that already provide this sort of help to people with mental health problems, such as the Wellbeing Enterprises group in Cheshire2. We will also consult people who have used mental health services and staff who work in them. We will see whether adding this support to people’s other ongoing care can be done in mental health services, whether we can evaluate it successfully, and whether it seems to be helpful for people.
The first stage of the study over the spring and summer 2016 will involve planning exactly what the Community Navigators support programme should consist of. We will set up a working group, which can help plan the programme, and stay involved throughout the study to monitor how it’s going and plan how best to evaluate it. The working group is using a co-production approach involving people with mental health problems, practitioners and researchers. We would like to involve up to five people who have personal experience of mental health problems in this working group. At working group meetings, we will provide information about possible ways the programme of support could work, and hear from experts in other organisations. Working group members will then discuss different options for the programme, and make their own suggestions or recommendations. We have set dates for five initial meetings of the working group in Central London.
Tuesday 26th April 2-5pm
Tuesday 10th May 2-5pm
Tuesday 31st May 2-5pm
Tuesday 14th June 2-5pm
Tuesday 28th June 2-5pm
Lived experience working group members will be offered payment for their involvement on the project (at a rate of £15 per hour) and travel expenses will be paid. We welcome enquiries from anyone who has experienced mental health problems. We would particularly welcome input from people who have: experienced depression or anxiety; have used specialist mental health services; and have some previous experience of being an advisor on a research project, or have worked as a researcher themselves.
For an initial discussion and more information about joining the Community Navigators Study Working Group, please contact the study researcher:
Kate Fullarton
tel: 020 7679 9051 k.fullarton@ucl.ac.uk
Please contact Kate by Friday 15th April.
- Campaign to End Loneliness: www.campaigntoendloneliness.org/
- Wellbeing Enterprises: www.wellbeingenterprises.org.uk/
OPEN ACCESS OF ALL PAPERS FROM APRIL 16
By Elvira Bramon, on 15 March 2016
All papers accepted for publication from 1st April 2016 will need to be OPEN ACCESS to be eligible for the new Research Excellence Framework.
We are required to deposit all our accepted manuscripts in the UCL depository from 1 April 2016. We cannot submit papers to the next REF unless they have followed this new open access rule. UCL will also be evaluated on our overall performance in making papers open access in this way. Of course, there is also an advantage to us of having our papers open access as more people can read them.
Here is a helpful summary written by Catherine Sharp, UCL lead on open access:
Open Access for UCL Psychiatry
The relationship between depositing manuscripts and creating a publication that is open access is complex. Catherine (contactable via openaccess@ucl.ac.uk) will respond to individual queries about this process if you can’t get advice locally.
Congratulations to Sonia Johnson winner of the Provost’s Teaching Award for Leadership in Education
By Elvira Bramon, on 9 March 2016
Sonia Johnson has been awarded the 2016 Provost’s Teaching Award for Leadership in Education. This is in recognition of developing and leading the new MScs in Mental Health Sciences Research and Clinical Mental Health Sciences at the UCL Division of Psychiatry. Sonia and the MSc teaching team provide an outstanding educational experience for our students. The course recruits talented students many of whom stay at UCL to do a PhD or clinical training. The research projects the students do supervised by UCL Psychiatry staff often get published in excellent journals.
Sonia thanked key colleagues in the MSc course including Vaughan Bell, Jo Billings, Chris Coup, Rebecca Jones, Gemma Lewis, Nuj Monowari, Nicola Morant and Sarah Rowe. More information on these prestigious awards here
http://www.ucl.ac.uk/teaching-learning/awards-funding/provosts-teaching-awards/winners-2016
Congratulations to Sonia and the MSc core teaching team!
1 in 10 suicide attempt risk among friends and relatives of people who die by suicide
By Jake Fairnie, on 10 February 2016
A study by Dr Ale xandra Pitman, Prof David Osborn and Prof Michael King (UCL Psychiatry), funded by the Medical Research Council, has found that people bereaved by the suicide of a friend or relative have a greater probability of suicide attempt than those bereaved by the sudden natural death of a close contact.
xandra Pitman, Prof David Osborn and Prof Michael King (UCL Psychiatry), funded by the Medical Research Council, has found that people bereaved by the suicide of a friend or relative have a greater probability of suicide attempt than those bereaved by the sudden natural death of a close contact.
Read the January 2016 paper in BMJ Open here: http://bmjopen.bmj.com/content/6/1/e009948.full
They also found that the probability of dropping out of a job or an educational course was higher in people bereaved by suicide, suggesting that employers and teaching staff should consider how to support people after a suicide (you can read more about this in the following Times Higher Education piece: www.timeshighereducation.com/news/dropout-rates-soar-those-affected-suicide ).
 The team analysed data from a national sample of over 3,400 adults aged 18-40 who had experienced the sudden death of a close contact. Of this sample, 31% had experienced a depressive episode since the bereavement, and 6% reporting having had to drop out from a course or job. Almost half (45%) the sample reported suicidal thoughts since the bereavement, and 6% had made a suicide attempt since the loss. To give a rough comparison with the general population in England, the 2007 Adult Psychiatric Morbidity Survey had shown that up to 21% of people in the equivalent age group had ever had suicidal thoughts in their life, and 7% had ever attempted suicide in their life. The UCL study figures of 45% and 6%, respectively, only related to the period since the bereavement – an average of only 4 years.
The team analysed data from a national sample of over 3,400 adults aged 18-40 who had experienced the sudden death of a close contact. Of this sample, 31% had experienced a depressive episode since the bereavement, and 6% reporting having had to drop out from a course or job. Almost half (45%) the sample reported suicidal thoughts since the bereavement, and 6% had made a suicide attempt since the loss. To give a rough comparison with the general population in England, the 2007 Adult Psychiatric Morbidity Survey had shown that up to 21% of people in the equivalent age group had ever had suicidal thoughts in their life, and 7% had ever attempted suicide in their life. The UCL study figures of 45% and 6%, respectively, only related to the period since the bereavement – an average of only 4 years.
The study authors had input from voluntary sector organisations providing bereavement support when piloting the questionnaire, including Cruse Bereavement Care, Samaritans, Widowed by Suicide, and Survivors of Bereavement by Suicide. Samaritans also advised on the wording of the press release accompanying the publication of this article, being mindful of the language used and avoiding any implication that suicide attempt might be inevitable after suicide bereavement. Read the Samaritans media guidelines on reporting suicide here: www.samaritans.org/media-centre/media-guidelines-reporting-suicide
– Click the following link for the press release for this study: www.ucl.ac.uk/news/news-articles/0116/270116-bereavement-suicide-attempt-risk/
– A statement from Samaritans about the study findings: www.samaritans.org/news/comment-study-bereavement-suicide-risk-factor-suicide-attempt-published-bmj-open
– A statement from Cruse about the study findings: www.cruse.org.uk/news/BMJsuicide
– If you have been affected by suicide, you can find a Public Health England resource called ‘Help is at Hand‘ at this link: www.gov.uk/government/news/you-are-not-alone-help-is-at-hand-for-anyone-bereaved-by-suicide
Winners of the UCL Big Christmas Switch Off Competition!
By Jake Fairnie, on 13 January 2016
 The DoP has won the UCL Big Christmas Switch Off Competition.
The DoP has won the UCL Big Christmas Switch Off Competition.
We have been announced as the Division with the largest proportion of staff and students pledging to switch off lights, appliances and equipment over the holidays.
Each year, a lot of lights, appliances and equipment gets left on over the holidays. And this a big financial and carbon impact. On Christmas day alone, UCL spends over £16,000 on energy.
This year we had the highest proportion of staff and students pledging to switch off over Christmas!… Find out more here: www.ucl.ac.uk/greenucl/get-involved/big-christmas-switch-off
Dementia patients in poor areas are 27% less likely to get help
By rejusro, on 30 November 2015
 A study by Dr Claudia Cooper (UCL Psychiatry) found that dementia patients in England’s poorest areas are 27 per cent less likely to be prescribed anti-dementia drugs than those in richer places. Read more in the Sun.
A study by Dr Claudia Cooper (UCL Psychiatry) found that dementia patients in England’s poorest areas are 27 per cent less likely to be prescribed anti-dementia drugs than those in richer places. Read more in the Sun.
Over 800,000 people in the UK have dementia and numbers are growing as people live longer. There is no cure but drug treatments can help, for example by slowing memory loss among some people. The 2009 National Dementia Strategy made fair access to these treatments a priority.
We investigated how likely it is that people living with dementia get these drugs. We looked at primary care records from 6% of the UK population, including 75,000 people with dementia, from 2002 to 2013. In England people from least deprived areas (generally the richest) were 25% more likely to be started on ‘anti-dementia’ drugs than people in the most deprived areas. This did not change over time despite the National Dementia Strategy and other government policies. By contrast, in Scotland, how deprived the area where people lived did not affect whether they got this treatment.
It is striking that people with dementia living in more deprived areas get less treatment in England but not Scotland. Scotland spends more on health than England and the countries have different health policies. One reason for this difference in dementia prescribing may be that from 2006 to 2009 NICE restricted prescribing of these drugs to people with moderate dementia but the Scottish Intercollegiate Guidelines Network did not. We think that people from more affluent areas may be more likely to ask for and get treatments not endorsed by guidelines. In addition, younger people with dementia were more likely to be treated than older people, and men were more likely to be treated than women.
More research is needed to help ensure that dementia treatment in England is fair and meets equalities targets. We should be aware that policies to restrict treatment availability probably affect people in deprived areas most and make sure that changes benefit everyone.
This work was supported by The Dunhill Medical Trust [grant number R296/0513].
 Close
Close


