Getting started: Community Navigator Study Working Group Meeting 1
By Kate C Fullarton, on 26 May 2016
On 26th April, a group of researchers from UCL and the McPin Foundation, people with lived experience of mental health problems and staff from the Complex Depression, Anxiety and Trauma (CDAT) service at Camden and Islington NHS Foundation Trust and the Complex Care Team (CCT) at Barnet, Enfield and Haringey NHS Mental Health Trust, came together for the study’s first working group. What is so exciting about this project, is being able to bring together people with such varied experiences, perspectives and expertise, to work out what the community navigator support should look like: What skills, qualities and experience should our community navigators have? How can they best support people to make social connections and access activities in their community? These are just some of the questions that we’ll try and come up with an answer to over the course of the project, and particularly in the next few months.
We began the session by looking at the initial plans for the study (click to see the presentation slides), before discussing the principles of co-production and how we could use these principles to inform how we work together as a group (click to read more about the co-production approach that we’re using in the study). We later had a whistle-stop tour through theories of loneliness and some existing projects such as Wellbeing Enterprises, Groups4health and Connecting People Study which helped us to begin thinking about the core elements of our model: what are we trying to target when we talk about loneliness? What methods do these existing projects use to help people feel less lonely? What tools can we use to begin talking with people about their social world? The most striking thing about this presentation, which can be accessed here , was the lack of research evidence outlining effective methods for reducing loneliness among people with mental health problems. This gives purpose to why we are doing this project and serves as a powerful motivator for designing the best possible model of support that we can.
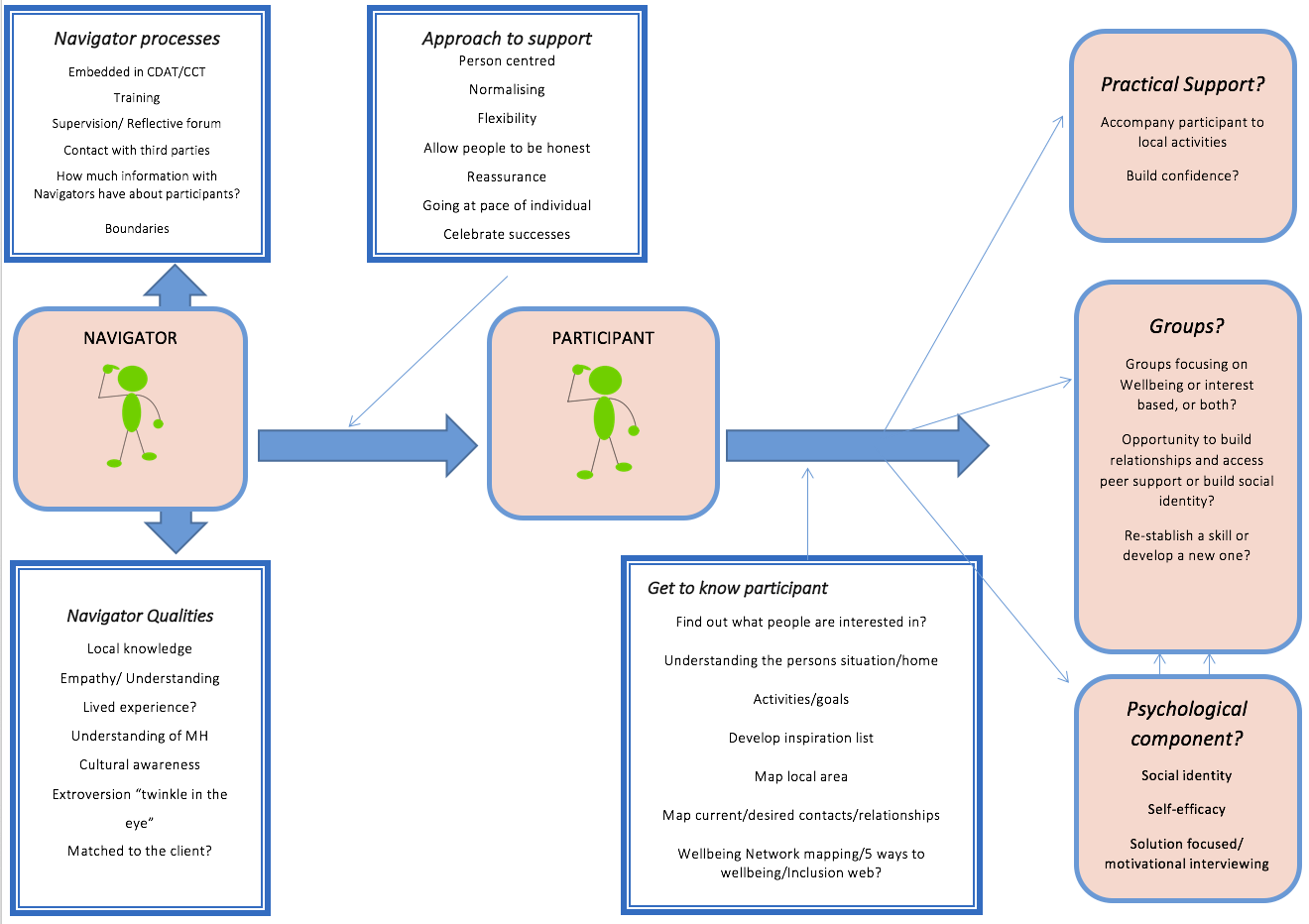
A particularly productive conversation resulted from everyone in the room splitting off into their primary group of expertise: practitioner, expert through lived experience or researcher. Each group was given a piece of flip chart paper and asked to put down their ideas for the community navigator support. We then came back together and discussed our ideas. These focused on the content of the support, the role of the community navigators and key questions which we’ll need to address before the community navigators’ work begins. What was interesting was that each of the groups came at this task from slightly different angles, reflecting their different perspectives of mental health services and providing a clear demonstration of how beneficial the co-production model will be.
This model illustrates the initial ideas the group had about the role of the community navigators and the support they will provide. What do you think? Is there anything that we’ve missed that should be added?
Despite really useful and animated discussions about community navigator support and the project more generally, we had run out of time and had to bring the first meeting to a close. Here, we’ve captured some reflections from people who attended:
“Healthy relationships are key to everyone’s mental wellbeing. Sometimes, traditional mental health ‘treatments’ don’t allow time to explore and address the other factors that are making a person feel isolated and lonely. Our communities often have rich untapped resources but that require some support to navigate. It is exciting to be involved in a project that is specifically working towards helping people to build social connections in a way that is meaningful to them.”
“I hope that our project will enable people like myself to begin to take their first steps forwards. For three years I struggled with agoraphobia, feeling frightened, alone and depressed, completely trapped in my isolation. One of my many hopes for our project is that we help more people like me to know that they are not alone.”
Another member of the group, working at Barnet, Enfield and Haringey (BEH) Mental Health Trust, said:
“At BEH we are delighted to be involved in this research project. Often loneliness is an issue under the radar of services despite the impact it can have on service users’ quality of life.”
We’ll be blogging again after our next meetings on 10th and 31st May. On 10th, we’re looking forward to hearing from Helen McPeake from Wellbeing Enterprises about the inspiring work they are doing in Merseyside and on 31st, Peter Bates , will be visiting to talk about his work developing training resources for staff in the National Development Team for Inclusion.
We’ll also be coming back to our model each week and seeing how what we’ve learnt can develop the model further.
If you want to know more about the study, please view our main webpage and check out the McPin blog.
Do you have any thoughts about the role of community navigators? Get in touch with Kate, the UCL researcher, by emailing k.fullarton@ucl.ac.uk.
 Close
Close


 xandra Pitman, Prof David Osborn and Prof Michael King (UCL Psychiatry), funded by the Medical Research Council, has found that people bereaved by the suicide of a friend or relative have a greater probability of suicide attempt than those bereaved by the sudden natural death of a close contact.
xandra Pitman, Prof David Osborn and Prof Michael King (UCL Psychiatry), funded by the Medical Research Council, has found that people bereaved by the suicide of a friend or relative have a greater probability of suicide attempt than those bereaved by the sudden natural death of a close contact. The team analysed data from a national sample of over 3,400 adults aged 18-40 who had experienced the sudden death of a close contact. Of this sample, 31% had experienced a depressive episode since the bereavement, and 6% reporting having had to drop out from a course or job. Almost half (45%) the sample reported suicidal thoughts since the bereavement, and 6% had made a suicide attempt since the loss. To give a rough comparison with the general population in England, the 2007 Adult Psychiatric Morbidity Survey had shown that up to 21% of people in the equivalent age group had ever had suicidal thoughts in their life, and 7% had ever attempted suicide in their life. The UCL study figures of 45% and 6%, respectively, only related to the period since the bereavement – an average of only 4 years.
The team analysed data from a national sample of over 3,400 adults aged 18-40 who had experienced the sudden death of a close contact. Of this sample, 31% had experienced a depressive episode since the bereavement, and 6% reporting having had to drop out from a course or job. Almost half (45%) the sample reported suicidal thoughts since the bereavement, and 6% had made a suicide attempt since the loss. To give a rough comparison with the general population in England, the 2007 Adult Psychiatric Morbidity Survey had shown that up to 21% of people in the equivalent age group had ever had suicidal thoughts in their life, and 7% had ever attempted suicide in their life. The UCL study figures of 45% and 6%, respectively, only related to the period since the bereavement – an average of only 4 years.








 UCL Psychiatry’s
UCL Psychiatry’s 
