UCL mental health research in older adults during COVID-19
By iomh, on 22 October 2021
By Dr Kathy Liu, MRC Clinical Research Training Fellow, UCL Division of Psychiatry
By the first national lockdown on 26 March 2020, many were aware that COVID-19 and related restrictions have a disproportionate impact on older adults and individuals affected by dementia. UCL mental health researchers responded rapidly to try to understand how older adult mental health and dementia wellbeing were affected and what should be done. This blog summarises some of the insights and research contributions we made.
Higher infection and death rates from COVID-19
An international study led by Dr Aida Suárez-González from UCL found that by August 2020, people with dementia made up around a third (31%) of COVID-19 related deaths in the UK1. The study group, including UCL researcher Prof Gill Livingston, linked this to high death rates in care homes where most residents have dementia. In the UK, older people were admitted to care homes without knowing if they had COVID-19 or not. These individuals were also often not allowed to access healthcare and were isolated and confined, with visitors to care homes banned.
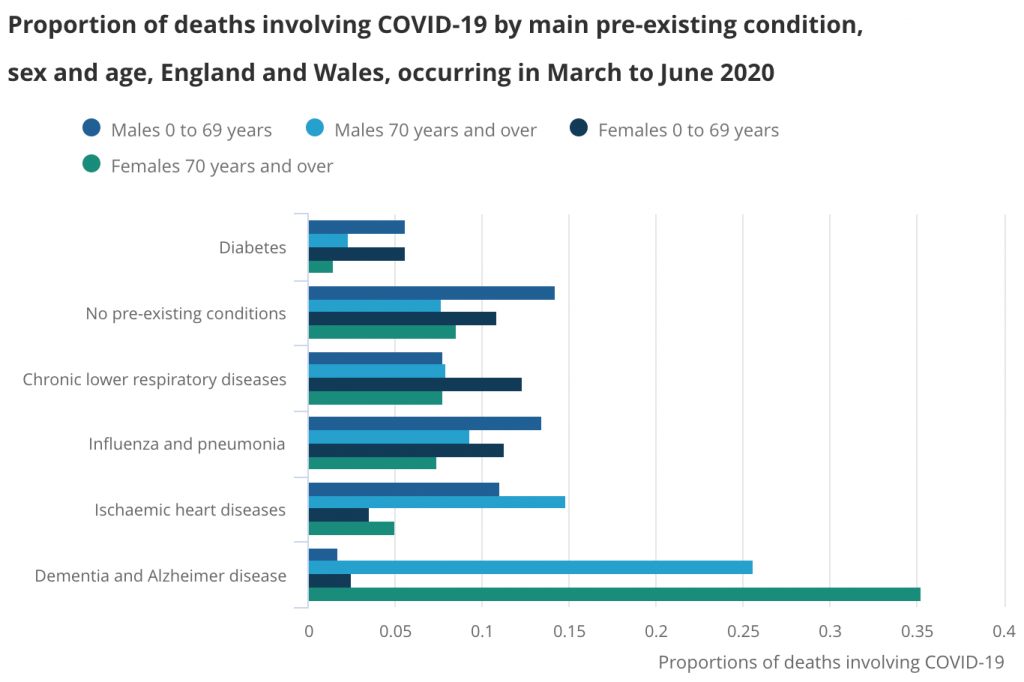 Dementia and Alzheimer disease was the most common main pre-existing health condition in deaths involving COVID-19 between March and June 2020. Published by the Office for National Statistics.
Dementia and Alzheimer disease was the most common main pre-existing health condition in deaths involving COVID-19 between March and June 2020. Published by the Office for National Statistics.
Negative impact of COVID-19 restrictions on dementia wellbeing
To assess the effect of COVID-19 isolation measures on people with dementia, Dr Suárez-González, Prof Livingston, and colleagues analysed findings from existing studies2. They found that isolation measures had a negative impact on memory and thinking and mental health, with almost all studies reporting a new onset or deteriorating distressing behavioural or psychological symptoms in people with dementia.
Increased prescribing to treat behavioural or psychological symptoms
Antipsychotic drugs can be used to treat distressing behavioural or psychological symptoms in dementia, such as agitation and psychosis, when non-drug approaches have failed. However, they have limited effectiveness and serious side effects. Prof Robert Howard from UCL led an investigation and found that rates of antipsychotic prescribing increased in people with dementia in England from March-July 20203. This highlights the need to monitor and reduce the rates of antipsychotic prescribing once COVID-19-related risks have decreased.
Monitoring COVID-19 infection and death rates in mental health hospitals
Infection control measures in hospitals are important to minimise COVID-19 infection and deaths in patients and healthcare staff. Prof Gill Livingston led a study including UCL researchers Dr Andrew Sommerlad, Dr Louise Marston and Dr Kathy Liu, and many NHS doctors, to measure infection and death rates in patients aged over 65 years or diagnosed with dementia between March-April 20204. Patients had been admitted to one of 16 psychiatric wards in NHS mental health hospitals in London. Data could be obtained rapidly as COVID research regulations allowed the use of anonymised hospital patient data without the need for individual consent, and regulatory bodies prioritised applications for such studies. The NHS doctors on the team also contributed their time and made efforts to help collect data rapidly. The study group found that mental health hospitals experienced a delay in accessing personal protective equipment (PPE) and COVID-19 tests compared to other hospitals. This likely contributed to higher infection (38%) and death (15%) rates compared to community levels, despite the government policy of parity of esteem for physical and mental health.
 Mental health hospitals experienced delayed access to PPE and COVID-19 tests during the first wave. Image by leo2014 from Pixabay.
Mental health hospitals experienced delayed access to PPE and COVID-19 tests during the first wave. Image by leo2014 from Pixabay.
After the study findings and recommendations were published, the research group repeated the measurements during the second pandemic wave between December 2020-February 20215. There were improvements in infection control measures and better outcomes for patients. Infection rates were lower (25%) with correspondingly fewer deaths. Vaccinations may offer additional protection against COVID-19 in future, but measures such as regular testing of inpatients remain appropriate, as a significant proportion of COVID-19 positive patients were asymptomatic (29%).
Reduced face-to-face approaches and adaptations by mental health services
UCL researcher Dr Rohan Bhome led a study6 to explore the perspectives of staff who worked in older adult mental health services between April and May 2020. The study highlighted areas that mental health services could develop to address staff and patient wellbeing during the pandemic. The team, including UCL researchers Dr Jonathan Huntley, Christian Dalton-Locke and Prof Gill Livingston, found that staff were concerned about barriers to infection control in hospitals and a lack of usual support for older people who lived at home. Staff responded positively to the shift to increased remote working but noted that some patients could not use the technology required for remote assessments.
 Staff working in older adult mental health services were concerned that some patients could not use the technology required for remote assessments. Image by Sabine van Erp from Pixabay.
Staff working in older adult mental health services were concerned that some patients could not use the technology required for remote assessments. Image by Sabine van Erp from Pixabay.
Negative impact on carers
Most family carers, including those caring for older people and individuals with dementia, are unpaid. Prof Gill Livingston was part of a team that published a report highlighting the impact of the COVID-19 pandemic on family carers7. Many carers increased their care hours during the pandemic. Access to support services, such as respite care and day centres, was severely restricted or more usually stopped. Some carers were also reluctant to continue with home care services due to concerns about the risk of infection. The report offered recommendations and policy considerations to improve outcomes for all carers.
 The wellbeing of carers was often negatively affected by the pandemic. Image by Gerd Altmann from Pixabay.
The wellbeing of carers was often negatively affected by the pandemic. Image by Gerd Altmann from Pixabay.
Directions for future dementia research
UCL researchers led by Dr Kathy Liu, with Dr Andrew Sommerlad, Prof Robert Howard and Prof Gill Livingston were part of a group that carried out a research update on dementia wellbeing during the COVID-19 pandemic8. The project was commissioned by the Department of Health and Social Care Dementia Programme Board. It incorporated findings from over a hundred studies on dementia wellbeing and COVID-19, using a framework published by NHS England (see figure below). From the findings, the group collectively identified key knowledge gaps to help researchers and organisations direct future research.
 Published by NHS England 2020
Published by NHS England 2020
Conclusion
UCL mental health researchers have worked rapidly to try to understand the impacts of the pandemic on older adults and individuals affected by dementia and make recommendations. Our future work will aim to explore and resolve outstanding research questions to improve the quality of life of these individuals and their carers.
REFERENCES
- Suárez-González, A. et al. Impact and mortality of COVID-19 on people living with dementia: cross-country report. https://ltccovid.org/2020/08/19/impact-and-mortality-of-covid-19-on-people-living-with-dementia-cross-country-report/ (2020).
- Suárez-González, A., Rajagopalan, J., Livingston, G. & Alladi, S. The effect of COVID-19 isolation measures on the cognition and mental health of people living with dementia: A rapid systematic review of one year of quantitative evidence. EClinicalMedicine 39, 101047 (2021).
- Howard, R., Burns, A. & Schneider, L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 19, 892 (2020).
- Livingston, G. et al. Prevalence, management, and outcomes of SARS-CoV-2 infections in older people and those with dementia in mental health wards in London, UK: a retrospective observational study. Lancet Psychiatry 7, 1054–1063 (2020).
- Liu, K. Y. et al. Infection control and the prevalence, management and outcomes of SARS-CoV-2 infections in mental health wards in London, UK: Lessons learned from wave 1 to wave 2. Undergoing peer review for publication (2021).
- Bhome, R. et al. Impact of the COVID-19 pandemic on Older Adults Mental Health Services: a mixed methods study. bioRxiv (2020) doi:10.1101/2020.11.14.20231704.
- Onwumere, J. et al. COVID-19 and UK family carers: policy implications. Lancet Psychiatry 8, 929–936 (2021).
- Liu, K. Y. et al. Dementia wellbeing and COVID-19: Review and expert consensus on current research and knowledge gaps. Int. J. Geriatr. Psychiatry (2021) doi:10.1002/gps.5567.
 Close
Close

