Inclusion Health: Co-producing a research and advocacy agenda
Chantal Edge, Dr Binta Sultan, Serena Luchenski, and Dr Al Story report on the launch of the UCL Collaborative Centre for Inclusion Health, funded by a small grant from UCL’s Grand Challenge of Justice & Equality.
There’s no avoiding the fact that health is getting worse for people who are at the extreme edges of society. The number of people sleeping rough has almost doubled nationally. Deaths among homeless people and people who use drugs are increasing, and we are putting more people in prison. This is driven by social and political forces. Over the last decade, austerity has led to record numbers of working families living in poverty and major increases in child poverty. Housing is unaffordable to millions, foodbanks have proliferated, children’s and youth centres have seen systematic disinvestment, and access to legal aid has been greatly reduced. At the same time, funding is decreasing for services which reduce the harms of extreme social exclusion, such as addiction treatment, needle exchange and hostels.
So what should we, as a multidisciplinary research and advocacy group, be doing to stem the tide of inequity? How can we stop people from becoming socially excluded, improve services for people who are, and ultimately help people escape exclusion? The team at our newly launched UCL Collaborative Centre for Inclusion Health has reached out to experts with lived experience of exclusion, policy makers, voluntary sector, health and social care workers and academics to frame our research and advocacy priorities for the next five years.
So what is Inclusion Health?
“Inclusion Health is a service, research, and policy agenda that aims to prevent and redress health and social inequities among the most vulnerable and excluded populations.” (Luchenski 2017, The Lancet)
Put simply, Inclusion Health is about understanding the forces that cause and perpetuate social exclusion so we can prevent it and bring vulnerable and under-served people in our society ‘out of the cold’. People who are homeless, drug users, prisoners, or sex workers suffer from poorer health outcomes than people in the general population and are far more likely to die early. Research at UCL found that women from these socially excluded groups were 12 times more likely to die than other women of the same age, and men eight times more likely. People who are socially excluded are more likely to be murdered or commit suicide and more likely to die from accidents, overdoses, infectious diseases, cancers, liver disease, heart problems and respiratory diseases. Social exclusion damages health, destroys lives and fractures communities. Dedicated research and advocacy to highlight the harms of exclusion and remedy the causes is urgently needed.
What is the new UCL Collaborative Centre for Inclusion Health?
The UCL Collaborative Centre for Inclusion Health (CCIH) was set up by a multidisciplinary team of researchers, experts with lived experience and frontline professionals who are dedicated to reducing health inequity. The Centre already has a broad range of research projects underway, measuring the health harms of exclusion and developing and testing interventions to improve the health of excluded groups. At the heart of all these projects are partnerships with people who have lived experience of exclusion (‘experts by experience’) and professionals from across the public and voluntary sector.
Co-producing the Inclusion Health agenda
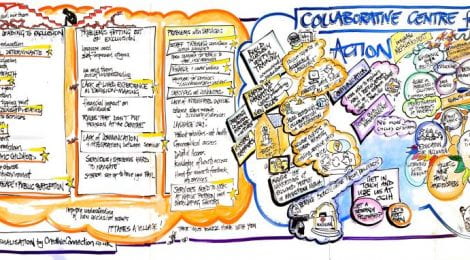
On 3 June 2019, the Centre held a launch event to bring together a wide range of experts to shape the agenda and co-produce research and advocacy priorities for the next five years. Over 100 representatives from the voluntary sector, policy, academia, healthcare and a wide range of experts by experience worked together to tackle three key areas – preventing exclusion, improving services for those who are excluded, and escaping exclusion. Through a series of presentations, workshops, democratic voting and ‘dream-boarding’ we collected and collated information on where we need to start.
Consultation and analysis is on-going but emerging priorities include:
- Tackling the upstream determinants of exclusion – political determinants, poverty and traumatic childhoods
- Addressing societal and professional ignorance, indifference and stigma that can further deepen and perpetuate exclusion
- Making services more accessible and integrated to stop people falling through the cracks
- Ensuring that experts by experience are at the heart of health research, service development and decision making
- Creating better routes out for people to escape exclusion
This event was run in partnership with the UCL Centre for Co-Production in Health Research and made possible by funding from UCL Grand Challenges, awarded to Chantal Edge and Niccola Hutchison-Pascal through GCJE’s Embedded Inequalities initiative.
Next steps
Over the coming months we’ll be disseminating our findings from the day. We will use this evidence to inform and influence research and advocacy priorities for funders, and ensure that our current and future research projects tackle the priorities that have been set.
There is a legal duty in England on politicians and policy makers to better integrate services and tackle health inequalities. People forced to the margins of our society suffer from humiliating disadvantage, preventable disease and premature death. Their lives, cut short, indicate that there is something toxic in our society. Evidence to inform better policy, practice and advocacy is urgently needed.
Chantal Edge is an NIHR Clinical Doctoral Research Fellow and Specialty Registrar in Public Health, researching the use of telemedicine for hospital appointments in prison. Dr Binta Sultan is an NIHR Doctoral Research Fellow and a Consultant in HIV and Sexual Health, her research centres on improving hepatitis C linkage to care in people who experience homelessness using novel technologies. Serena Luchenski is an NIHR Clinical Doctoral Research Fellow, a Consultant in Public Health and Chair of the UCL Collaborative Centre for Inclusion Health; her research is on developing a public health preventative approach to hospital care for people experiencing homelessness. Dr Al Story leads the Find&Treat Outreach Service based at UCLH and is Co-Director of the UCL Collaborative Centre for Inclusion Health.
If you’re interested in learning more about Inclusion Health more information is available here. If you are interested in becoming involved in Inclusion Health research please contact ccihcore@live.ucl.ac.uk outlining your area of interest.
This article was originally posted on the IEHC blog and can be accessed here.





Comments are closed, but trackbacks and pingbacks are open.