Regenerative medicine: is the grow-your-own organ era just around the corner?
By news editor, on 10 June 2013
![]() Written by Emily Burns, who attended a lecture by Professor Martin Birchall (UCL Ear Institute) at the Cheltenham Science Festival, entitled ‘Regenerative Medicine: Where will we be in 50 years?’
Written by Emily Burns, who attended a lecture by Professor Martin Birchall (UCL Ear Institute) at the Cheltenham Science Festival, entitled ‘Regenerative Medicine: Where will we be in 50 years?’
What happens if a newt’s leg is cut off? Or a gecko’s tail auto-amputated?
The cells simply multiply to grow back into exactly what was missing. If a flatworm were cut in two, the two halves would both become new flatworms.
Unfortunately for humans, this incredible ability to self-regenerate was lost several branches ago on the evolutionary tree. As such, we definitely don’t have the ability to grow a new leg, or a new heart.
We have to rely on skin grafts and organ transplants, with common risks of rejection, infection and multiple complications. However, according to Professor Mark Birchall and Dr Felicity Mehendale, our regenerative future is just around the corner.
Organ transplants are a logistical nightmare for patients and doctors: long waiting lists; poor quality organs; the risk of a life on debilitating immunosuppressant drugs is often inevitable. But this may all soon change, with the arrival of new technologies that allow stem cells to be grown into organs.
Human stem cells can be expanded in the laboratory into the specific cells that we need – such as heart muscle or epithelial cells – using a cocktail of growth factors. In 2010, Professor Birchall was part of the team that gave a young boy a new trachea, built from his own stem cells onto the collagen skeleton of a donor trachea. It was hoped that this groundbreaking procedure would reduce chances of rejection, as the stem cells wouldn’t induce an immune response. It worked, and it’s just the beginning.
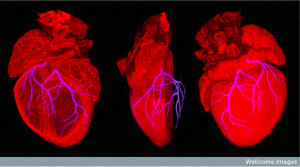
Huge advancements have been made in the field: Harvard has developed a lung that ventilated a rat, while Yale has developed a kidney for a rat that produced urine for eight hours. Stem cells can now be layered onto a collagen scaffold in the shape of the desired organ. Specific growth factors and signalling chemicals are added, allowing them to differentiate into the right cell type and build up into the organ that’s needed. It’s even possible (although still at the extremely early stages) to 3D print stem cells onto biopaper that degrades once the cells have adhered together, opening up possibilities for growing organs without even the need for a scaffold. While there’s still a long way to go, portions of cardiac artery have been created and transplanted already.
It’s incredible to think of how far we’ve come since the London Tin Noses Shop of World War I, where sculptors were used to fashion prostheses out of tin. Instead of tin masks and Gillie’s tubed pedicle, we can seed the collagen scaffold of an ear with stem cells in order to grow another one.
It is important to remember here that humans can regenerate the epidermis (top layer of the skin), but the dermis underneath must be present. This poses a problem for skin that is grown in the laboratory: the dermis must be present as a scaffold. This often isn’t the case – in burn victims, for example – so artificial scaffolds can now be used.
Is it possible that there could be a 21st century Tin Noses Shop, complete with living biocompatible tissue? The pharmaceutical industry isn’t too interested just yet, but hopefully the first few trials will grab attention and investments. At present, we don’t know the long-term effects of the surgery and regenerative medicine involved in these procedures. It can therefore only really be used as a way to treat end stage disease when there aren’t any other options.
While randomised clinical trials are the standard procedure, they won’t be beneficial in rare – and often unique – conditions. The risks associated with putting stem cells back into a patient (such as the possibility that they will differentiate into another unwanted cell type) are currently unknown. Scientists and doctors must wait and see what happens with the small number of procedures that have been carried out so far.
Christopher Reeve, who was paralysed after falling from a horse in 1995 and died in 2004, was a strong advocator of stem cell research. In 1996, he said: “So many of our dreams at first seem impossible, then they seem improbable, and then, when we summon the will, they soon become inevitable.” While at the first stages of development, it is clear that these regenerative techniques using stem cells are the inevitable and incredibly exciting future of medicine.
Emily Burns is a UCL PhD student working in the Structural Biology laboratory at the London Research Institute.
 Close
Close