Read this before developing an mHealth app: tips on saving time and money by walking in other people’s shoes
By Marilia Duque E S, on 15 September 2020

An example of a desire path, a consequence of erosion due to people walking on it rather than taking the pre-designed path. Photo licensed under the Creative Commons Attribution 2.0 Generic license
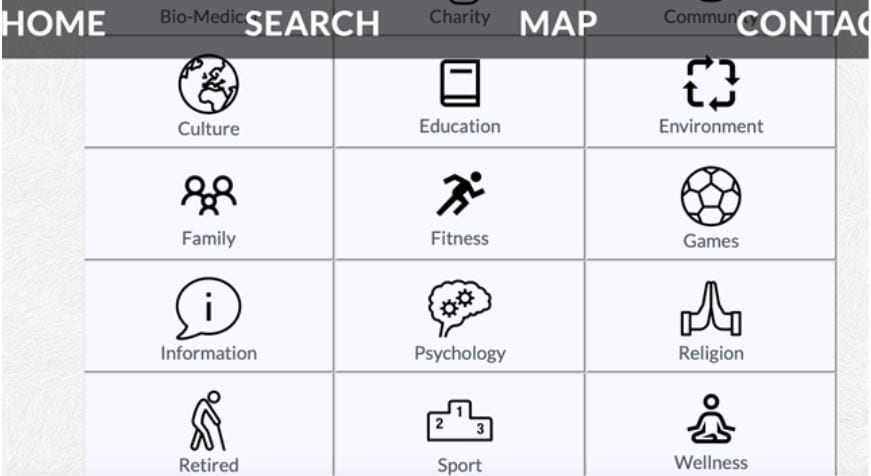
A few weeks ago, I was invited to mentor a startup. They used the term mentorship, but it was more like an informal talk. They are developing an app to help relatives coordinate the care of their elderly parents. Their motivation for this is genuine. The founders are three siblings who had a hard time when they found themselves having to take care of their mother, who had dementia, for several years. They believe they have learned a lot from their experience and they could help other families by combining all the resources they needed as caregivers into a single app. They did a great job. The app is a combination of a calendar for medication and doctor’s appointments, a chat feature the family can use to talk, a channel for checking health information, another channel that can be used to connect with doctors and caregivers and a function that provides reliable, trustworthy information and medical guidance. They also invited one of the most respected researchers on health and ageing to support them with the development of this tool. So, why do I think this app might fail?
During the ASSA project, I conducted a 16-month ethnography with older people in Sao Paulo. At the beginning of fieldwork, I was expecting to find people using apps specifically designed for health and care. Instead, I found people using WhatsApp to create groups to coordinate the care of relatives and to get medical guidance from friends. WhatsApp is the main means of communication among Brazilians who own a smartphone, so the decision to place conversations addressing health and care onto the platform seems natural, especially among older people, as sometimes, WhatsApp is the only app they feel comfortable with. Centralising multiple tasks on WhatsApp means they don’t have to install a new app. This is relevant because, due to many older people using a second-hand device, mobile phone memory can be a problem. Moreover, the process of downloading an app is itself one of the things that they find can make them feel like they have got stuck. Even if they succeed in downloading a new app, they may face constraints related to the adoption of new technology. As one of my research participants said: “you don’t change a winning game”. They just feel like they are at home when they are using WhatsApp.
That is not the case of the three startup founders I am talking about. They are young and technology is not a barrier to them. However, most of the siblings I met who were taking care of elderly parents were middle-aged. This demands an exercise of empathy, which is not just about identifying what caregivers need. It is crucial to consider where they would like to find what they need. It is important to learn how and where (in which app) they get things done. The eureka moment should then come when developers understand how to improve and add value to the choices the users have already made. Katrien Pype called this ‘smartness from below’[1].
In my research, I work with the term “desire path”[2]. In a park, for example, the desire path is the path users create by choosing a route that is different from the one designed by planners. The desire path is the materialisation of the free will. It can be seen as a kind of disobedience, but there is something really valuable about this unpredictable preference. Observing the desire path is an opportunity to learn what users feel is more appropriate for the experience they want. In that sense, taking the desire path into account can save resources and time and might be a good short cut to succeeding in the challenge of designing an app people are actually willing to use.
Because the app they are planning to develop contains an in-built calendar, one of the questions I asked the startup’s founders was whether they would normally use a calendar other than Google. They said they wouldn’t. So why assume their users would use something different to what they are used to? It is easier to integrate the schedule that caregivers need to keep track of the care they provide (sometimes across multiple family members) into the calendar they already use in their day to day life, rather than persuading them to adopt a new one. In that case, Google Calendar is the desire path and app developers are the ones who should adapt their journey to the use of it. The same occurs with WhatsApp. Based on this experience as well as my observations during fieldwork in Sao Paulo, investigating how doctors, clinics and insurance health plans in the city were using WhatsApp for health purposes, I developed a series of protocols for clinics and hospitals showing how WhatsApp can be used to facilitate their communication with patients when it comes to patient triage, the provision of medical care and patient education. These protocols were published under the title “Learning from WhatsApp: Best Practices for Health” (you can download this for free here). In the 150 pages of the book, I haven’t invented anything. It is just simple and pure WhatsApp. My work was to learn with people and systemise the steps.

Figure 1: Example of how WhatsApp might be used to coordinate remote care. In this case, the nurse in charge of interacting with patients via Whatsapp uses the ‘star message’ function to indicate that the patient’s query is pending, so she can go back to the patient after the image is seen by the doctor. Source: ‘Learning from Whatsapp: Best Practices for Health’, by Marilia Duque.
I also published another book called “WhatsApp for Nutritionists” (the book was only published in Portuguese and it is available here). The book is a result of a project I worked on where my challenge was to rebuild the kind of food diary[3] a bespoke m-Health app provides but using only WhatsApp features. The intervention’s effectiveness was tested by having older people assisted by the UNIFESP Medical School in Sao Paulo trial the new method. Participants were invited to take a picture of everything they ate and drank every day and shared this with the nutritionist via WhatsApp. They didn’t have to learn anything new and neither did the nutritionist, as both were already WhatsApp users. This way, the medical school didn’t have to develop an additional app in order to create a reliable method for assessing dietary requirements and needs. It was a successful and cost-effective intervention.


Figure 2 and 3: Examples of how Whatsapp can be used for nutrition purposes – the user sends the nutritionist a photo of all of their meals, thus creating a visual log of their nutritional intake for the day. These are examples of how nutritionists can visualise a patient’s food diary on their mobile and on WhatsApp Web. Source: WhatsApp® Aplicado à Nutrição, by Marilia Duque.
I do think the app I was invited to talk about is far better than WhatsApp, and it should be, as it was designed specifically for health purposes by people who have experience in the problem they want to solve. My point is that there is no guarantee people will use it. That is why my advice is to observe, learn and respect the desire paths taken by potential users before developing something new. They are the choices people have already made.
[1] Pype, Katrien. “Smartness from Below: Variations on Technology and Creativity in Contemporary Kinshasa.” What Do Science, Technology, and Innovation Mean from Africa?, edited by Clapperton Chakanetsa Mavhunga, The MIT Press, 2017, pp. 97–115.
[2] https://www.theguardian.com/cities/2018/oct/05/desire-paths-the-illicit-trails-that-defy-the-urban-planners
[3] RUCKENSTEIN, M. (2015). Uncovering Everyday Rhythms and Patterns: Food tracking and new forms of visibility and temporality in health care. Techno-Anthropology in Health Informatics: Methodologies for Improving Human-Technology Relations, 215, 28-40.
 Close
Close