We kicked off our second working group meeting by reflecting on the model that we began building in our first session. It was a useful reminder of how much was achieved in just a single meeting, and provided a framework on which to build.
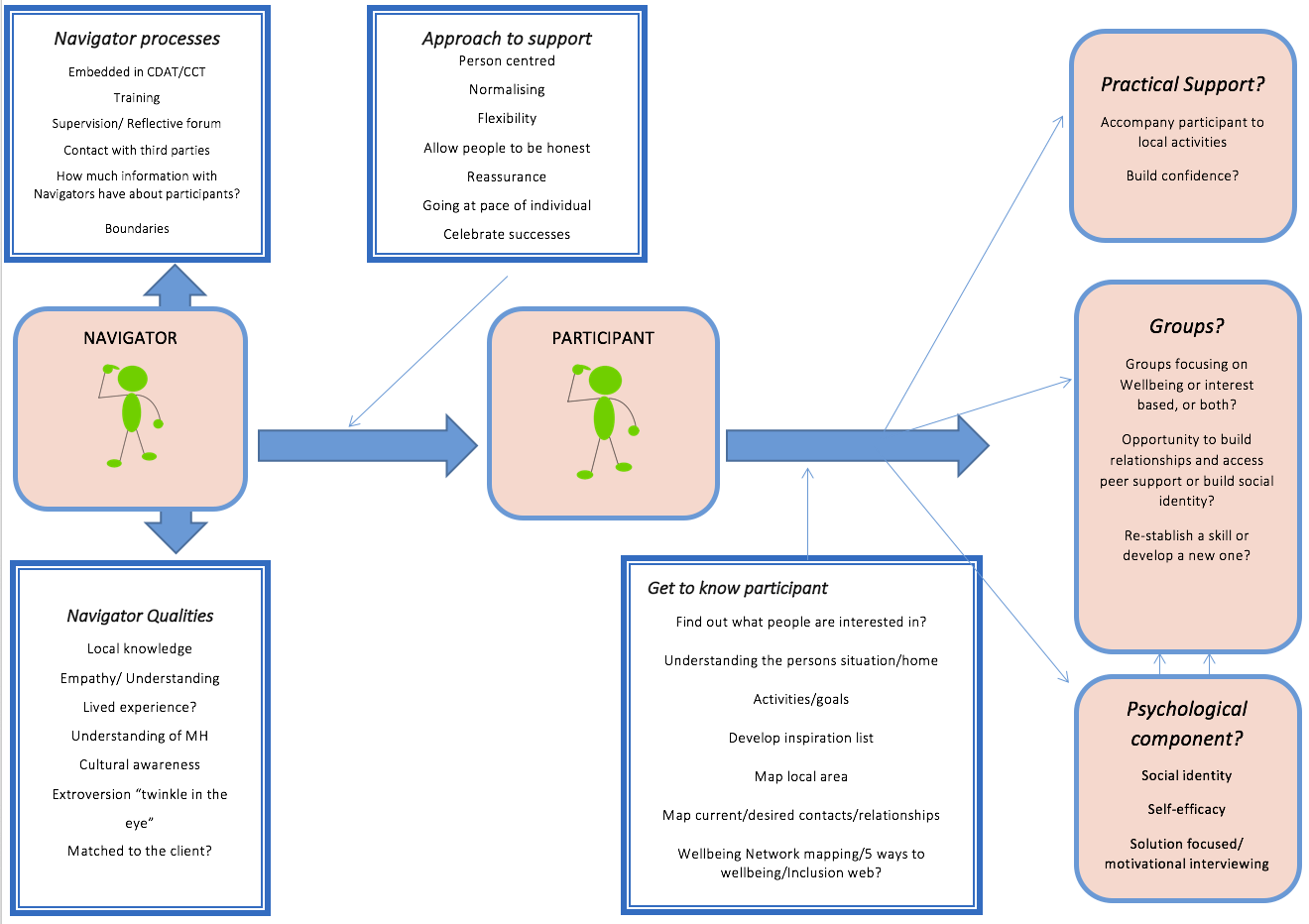
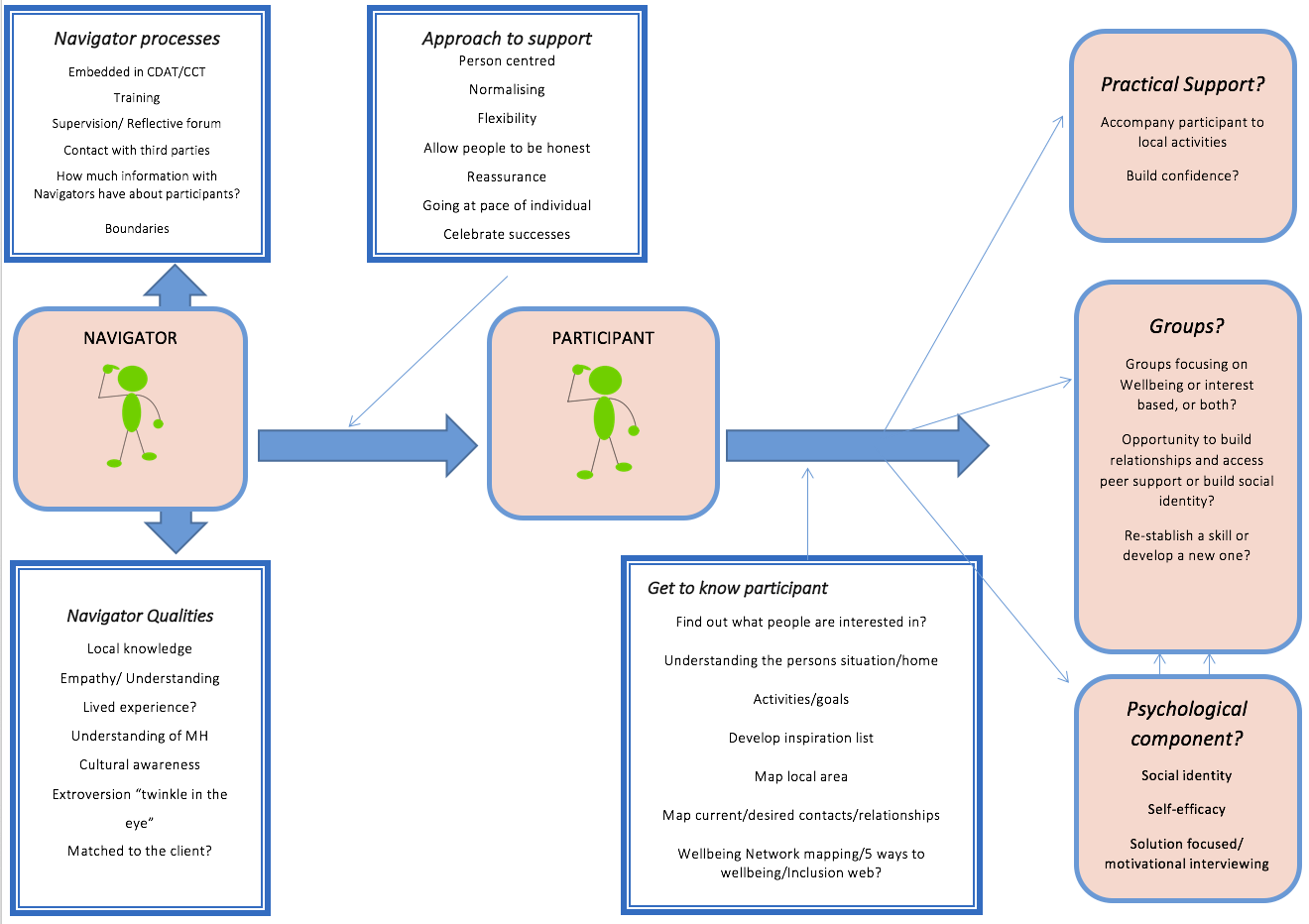
Model from Week 1
We then heard from Helen McPeake, a Senior Project Manager from Wellbeing Enterprises (WE), an organisation based in Merseyside, which works to improve the health and wellbeing of local communities, by tackling loneliness and isolation. The interest and engagement in WE’s work was clear, prompting questions from around the room. Helen answered all of our questions and we gained a very clear sense of the WE model.
WE have Community Wellbeing Officers based in GP practices who work with people to empower them to ‘talk’, ‘connect’ and ‘take action’. The wellbeing officers focus solely on social issues, helping service users improve social support and access groups and services. This process begins with a ‘wellbeing review’, which lasts around forty minutes and allows people to talk about what is bothering them and what they might like to be doing more of in their lives. The Wellbeing Officer then works with the person to set goals around connecting with practical support, services, activities and other people in the community. The Wellbeing Officer may also refer people to ‘Social Prescribing Programmes’ which are short courses available through WE. After three, nine and twelve months, the Wellbeing Officers meet again with people or arrange telephone follow-ups.
Learning more about WE and the impact they have had in their community was inspiring for us all. One of the big questions we had for Helen was how she saw this working for people who are using secondary mental health services for persistent anxiety or depression and perhaps have more complex needs. What was particularly inspiring was hearing Helen describe the WE ethos as truly person-centred and the ‘can do’ attitude of WE practitioners, consistently reassuring us that it doesn’t matter about a person’s diagnosis or their past, but about what can be done now. A phrase that kept coming up was ‘What is the most important goal for you right now?’
As she spoke, a palpable feeling of optimism grew around the room, and after a short break, we began to capitalise on all the ideas that her talk had sparked. We divided ourselves into pairs and on a copy of the model from the first meeting, added, changed or removed anything from the model as we felt was needed, before discussing these ideas as a group.
Comparing our work from the first and second meetings, it’s exciting to see how our model is developing as new ideas are added. We’re also coming up with lots of questions about what exactly the community navigator support should look like, which we’ll definitely be returning to.
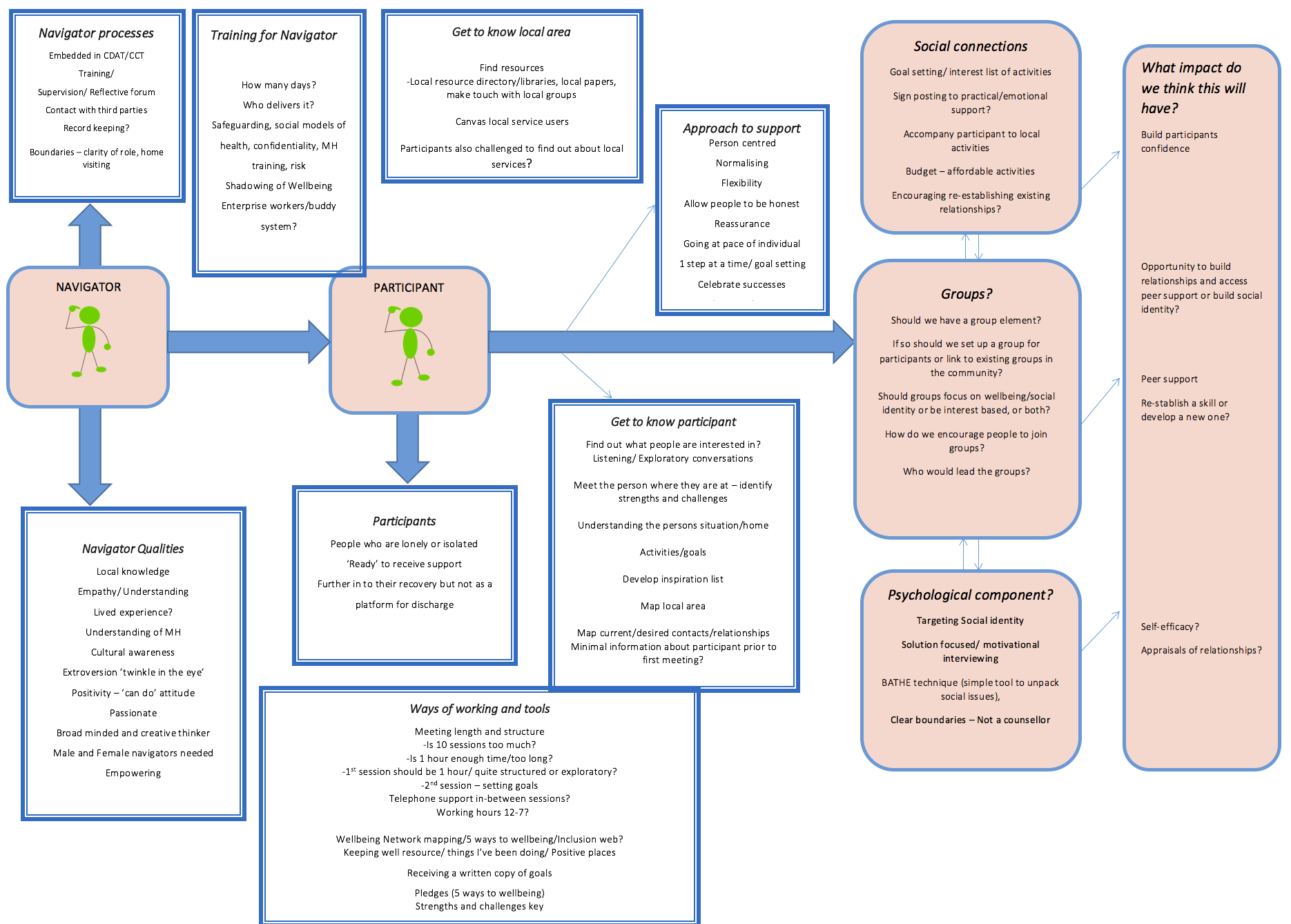
Model from Week 2
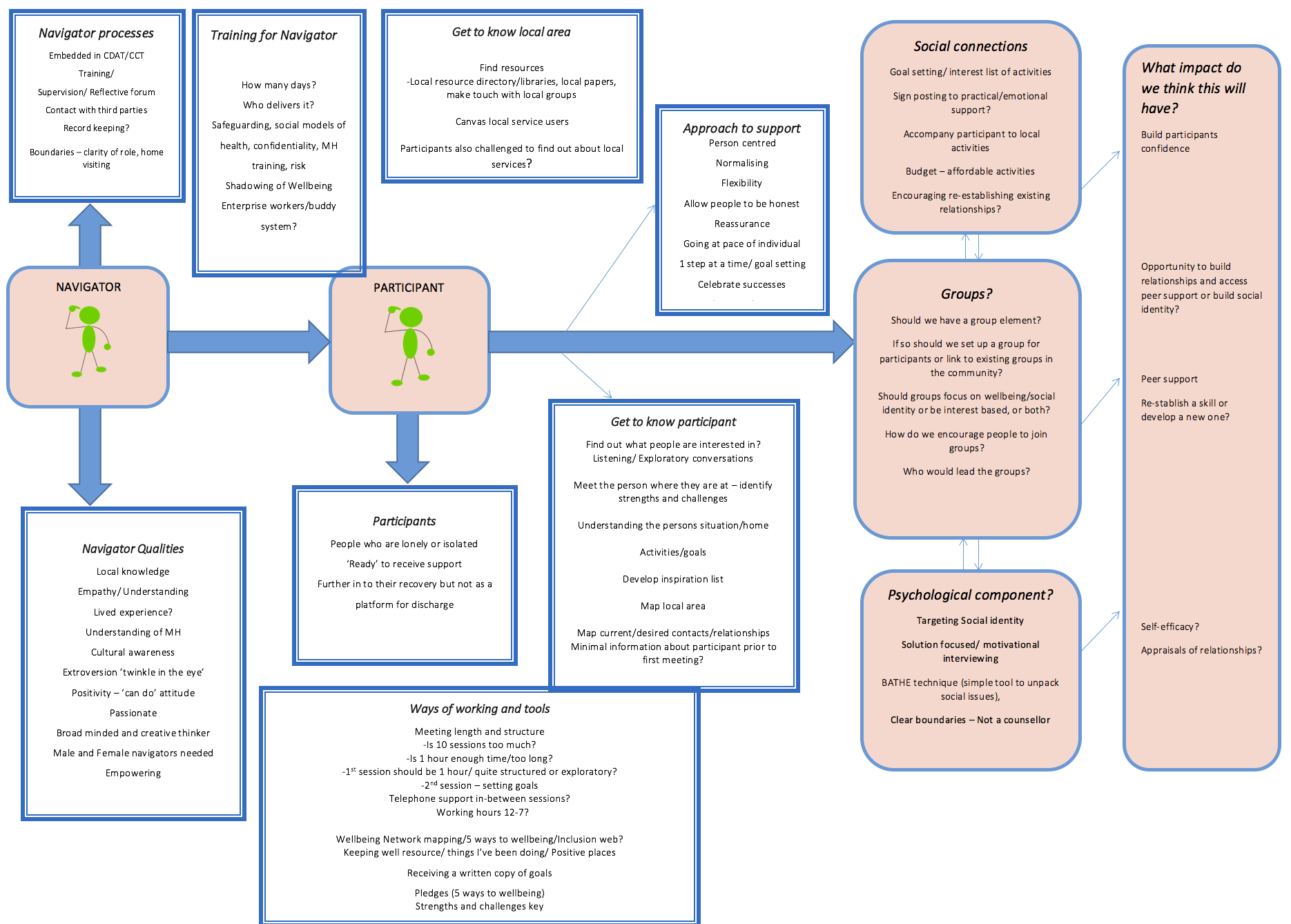
Some of these questions include: should we be connecting participants to pre-existing groups in the community or should we be setting up our own groups for participants to attend like Wellbeing Enterprises have? If so, should these be well-being focused groups, such as mindfulness, or should they be more activity based and interest-led? The various benefits and drawbacks of these approaches were discussed, and we’ll come back to these ideas in future weeks as we begin to make decisions about the programme of support. Another question that came up was the length and structure of sessions over the six months that participants receive support from a community navigator. Helen explained how much could be achieved in relatively fewer and briefer sessions, when they are clearly structured, but would this work for people with complex needs? What are your thoughts? Is 10 sessions over a 6 month period too much? Or perhaps it’s about right, or not long enough?
We’ve also created a new column, on the right hand side of the model, headed ‘What impact do we think this will have?’ This is to make sure we that when we make decisions about what the community navigator support includes, we are basing this on a clear rationale about why we think that element will reduce feelings of loneliness.
Bringing us back to reality a bit, we then heard from one of the practitioners on our working group, who discussed the current challenges to delivering this type of support within a secondary mental health service setting, reminding us of the context the Community Navigators will be working in. There does seem to be real enthusiasm for the Community Navigator role amongst the participating services, however, and a strong sense that this type of support should be beneficial to service users, so the atmosphere of optimism was not diminished.
As this meeting was nearing its end, we then turned to Bryn, one of the co-leads on the study to discuss the Community Navigator job advert. This is now live, so if you’re interested, take a look, and apply here.
We’ll next be blogging after our meeting on 31st May, when we’ll hear from Peter Bates, who will be visiting to talk about his work alongside the National Development Team for Inclusion.
Until then we would love to hear your thoughts on our key questions. These include:
Should the support include a group aspect? If so, what type of group? Should we be targeting the psychological aspects of loneliness or focusing on helping increase social activities?
Get in touch with your thoughts on Twitter or get in touch with Kate, the UCL researcher, by emailing k.fullarton@ucl.ac.uk.
If you want to know more about the study, please view our main webpage.
 Close
Close