Mental health and wellbeing after humanitarian emergencies: what do we know about support programmes for children and young people in low- and middle-income countries?
By UCL Global Youth, on 6 November 2017
To celebrate Humanitarian Evidence Week (6-12th November), we have a guest blog post by Kelly Dickson and Mukdarut Bangpan, EPPI-Centre, Social Science Research Unit, UCL Institute of Education
 The United Nations Children’s Fund estimate that a quarter of the world’s children are living in countries affected by conflict or natural disasters. We know that these events can have a long-term impact on children’s and young people’s mental health and psychosocial wellbeing, and while many programmes have been designed to support children and young people dealing with the consequences, our knowledge of what works and why is still developing. To address this gap, Oxfam and the Feinstein International Center humanitarian evidence programme, commissioned us, as part of a wider review, to draw together a synthesis of outcome evaluations from across the world to gain a view of research effort in this area. Our review sought to capture the full range of approaches taken to provide mental health and psychosocial support (MHPSS) for children and young people (CYP) in countries affected by conflict or natural disasters, and the outcomes they seek to improve.
The United Nations Children’s Fund estimate that a quarter of the world’s children are living in countries affected by conflict or natural disasters. We know that these events can have a long-term impact on children’s and young people’s mental health and psychosocial wellbeing, and while many programmes have been designed to support children and young people dealing with the consequences, our knowledge of what works and why is still developing. To address this gap, Oxfam and the Feinstein International Center humanitarian evidence programme, commissioned us, as part of a wider review, to draw together a synthesis of outcome evaluations from across the world to gain a view of research effort in this area. Our review sought to capture the full range of approaches taken to provide mental health and psychosocial support (MHPSS) for children and young people (CYP) in countries affected by conflict or natural disasters, and the outcomes they seek to improve.
What did we find?
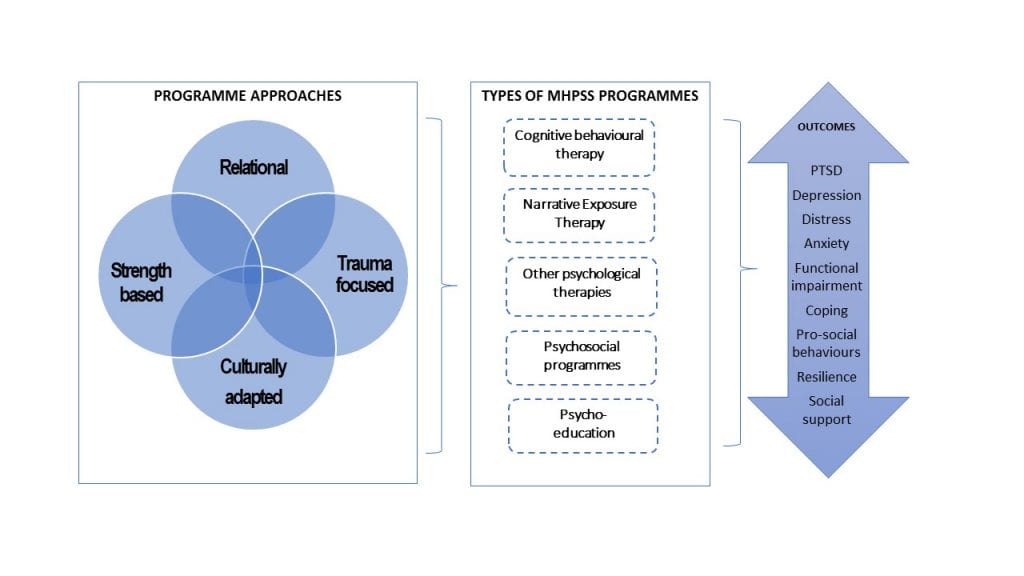
We found that evaluations of MHPSS programmes for children and young people are still relatively new with few conducted before 2004, and most appearing in the last five years. A rich diversity of approaches are currently being tested for their efficacy, measuring a wide range of outcomes. For example, programmes might incorporate trauma-focused approaches e.g. using psychological techniques tailored to meet the needs of CYP experiencing emotional and psychological difficulties or take a strength-based approach, focusing on CYP’s individual resilience and family and social networks to develop positive coping strategies.
Common psychotherapeutic modalities such as cognitive behaviour therapy or narrative exposure therapy were most likely to address and measure mental health outcomes such as post-traumatic stress disorder, depression, functioning or anxiety. They also measured psychosocial outcomes such as pro-social behaviours (e.g. actions which benefit someone other than yourself) and, less frequently, hope and resilience. Psychosocial programmes were similarly ambitious in their aims, measuring a range of both mental health and psychosocial outcomes.
Figure 1 Types of programmes and outcomes measured
Of the 45 MHPSS programmes identified in our review, many took advantage of whole-school or classroom-based settings to deliver programmes to children and young people in groups rather than 1:1 settings. Although not possible to outline each programme in detail, two case examples, indicative of the need for support, programme components and outcomes measured in the field, are provided below:
MHPSS after the 2008 earthquake in Sichuan province, China
A large number of young people were exposed to the harrowing events of the 2008 earthquake in the Sichuan province, China. Many of those who survived showed signs of being extremely fearful and anxious and went on to develop psychological problems, such as post-traumatic stress disorder (PTSD) and depression. In 2010, a short-term (six sessions) group cognitive behaviour programme was designed to support adolescents, who had lost one or both parents, manage trauma-based fears and negative thought patterns. The programme aimed to teach young people relaxation techniques and imagination skills, such as finding a ‘safe place’ in their mind. They were also supported to cope with intrusive flashbacks through guided meditation and nightmares through dream intervention exercises.
The programme needed to be adapted from the original manual (‘Children and Disaster: Teaching Recovery Techniques’, initially developed by the Norway, Foundation for Children and War) to ensure it was suitable to a Chinese context. Firstly, by removing exploration of avoidance behaviours, as they are often viewed as important adaptive strategies, to help people cope with change. Secondly by including the use of culturally specific examples of how to view events, ideas and emotions in a more positive way (cognitive re-framing). The aim of the programme was not only to ameliorate symptoms of PTSD and depression, but also to provide young people with the psychological resilience to recover and thrive as they made the transition from adolescence to adulthood.
MHPSS in conflict-affected contexts
War affected communities in the Democratic Republic of Congo continue to live under constant threat of attack and/or abduction by militia operating in the region. Growing up in armed conflict settings can destabilise familial relations and lead to emotional and behavioural difficulties in children and young people. To improve CYP’s mental health and psychosocial outcomes, (such as PTSD, conduct problems, prosocial behaviours) a family focused, community-based psychosocial intervention was designed for children aged 7–18. Programme activities included: psychoeducation about the impact of war, a life skills leadership course, relaxation techniques and mental imagery exercises, effective communication and conflict resolution skills and short video clips to address discrimination and stigma towards former child soldiers who had returned to the community.
Programmes activities were adapted to be culturally familiar to the local population by using culturally familiar songs, games and rituals, and drawing on local cultural and spiritual beliefs about how to address MHPSS well-being. The programme was also highly relational, focusing on building positive and trusting relationships with young people and enhancing community ties. Programme providers sought to encourage positive family interactions and community acceptance through these approaches to help mediate and improve the mental health and psychosocial of war affected youth.
Theory as a missing link
However, despite these efforts to build an empirical evidence base, studies commonly lack an explicit description of the programme theory underpinning their design. Further theorisation on the links between programme aims and focus, choice of programme components, delivery and anticipated mechanisms for improving outcomes for CYP could provide a more nuanced understanding of how and why MHPSS may or may not work. This programme theorization could also benefit from an understanding of how characteristics of young people, such as age, gender or other individual or social characteristics also interact with and mediate the impact of programmes in natural disaster and war affected settings.
 How did we get these findings?
How did we get these findings?
We conducted a comprehensive search of 12 bibliographic databases and 25 websites. We included studies published in English from 1980 onwards, if they delivered MHPSS programmes to one group of children in LMIC and compared their findings against another group of children who did not participate in a programme. To find out more about the systematic review and evidence on the effectiveness of programmes, please see the evidence summary of the full report here.
Acknowledgements
The research was funded by The Humanitarian Evidence and Communications Programme (HEP), a partnership between Oxfam and the Feinstein International Center, Tufts University on behalf of the Department for International Development. To find out more about the systematic review and evidence on the effectiveness of programmes, please see the evidence summary of the full report.
One Response to “Mental health and wellbeing after humanitarian emergencies: what do we know about support programmes for children and young people in low- and middle-income countries?”
- 1
 Close
Close




thanks for info