Reconstructing Broken Bodies: From Industrial Warfare to Industrial Engineered Tissues
By zclef78, on 5 July 2014
An illuminating and occasionally gruesome lecture for a non-medic unused to the visual realities of war, the third of the series UCL Lunch Hour Lectures on Tour marking the centenary of the First World War tackled a rarely discussed aspect of the aftermath of trench warfare.
The idea of the fabrication of living tissues to repair injuries is well publicised in the media today, from growing an ear on the back of a mouse, to full face transplants.
However, the development of reconstructive techniques was largely precipitated by the industrial scale of conflict in WW1.
Sadly, Professor Robert Brown (UCL Surgical Science) was unable to attend, so we were left in the capable hands of Colin Hopper (UCL Eastman Dental Institute) who delivered both the historical and medical sides of the lecture with distinctive candour.
Early medical advances
I was unconvinced that a GCSE in Biology would get me through the finer points of tissue fabrication, so it was a relief that we began with the historical context of medical advances during military conflicts since the early 1800s.
The fact that disease was responsible for a large number of deaths during the wars between 1804-15 was hardly a surprise, but the scale of the death–nearly 266,000 of the 311,806 deaths (85%) in the Army and Navy–showed just how much of an impact developments in medicine made to survival rates in future conflicts.
Changes in strategy and weaponry in WW1 caused a significant increase in the number of soldiers who sustained head and limb injuries, yet over 92% of wounded British soldiers evacuated to British medical camps survived. Some fairly horrific slides of facial injuries from more recent Iraqi and Libyan conflicts demonstrated the consequences of the types of weaponry used a hundred years earlier. Major General Henry Shrapnel has a lot to answer for.
As a head and neck surgeon, Colin was interested to know how much the audience thought a person needed of their face to survive. Drawing a line running from the top of the head and behind the ears with his hand, he revealed that anything below that line is an “optional extra”–who needs frontal lobes?
Head, shoulders, knees and toes
There were other early developments in medical practices that greatly improved the chances of surviving WW1. With the advent of the Thomas Splint, the mortality rate for a leg fracture dropped from 80% to 20%. Dominique Jean Larrey had already established the concept of triage, and thanks to Lister we had antiseptic.
Once we captured a few German pilots we also discovered Kuntscher’s nail system to fix femoral fractures, allowing airmen to return to active service within six weeks. Ilizarov in Russia developed a frame system for fixing mal-unions in fractures, but his technician accidentally turned the screw the wrong way and found that instead he could grow limbs.
Al Capone, The Guinea Pig Club.
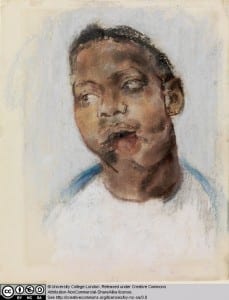
Colin then focused on the work of several prominent surgeons and doctors from WW1 onwards, amongst them Sir Harold Gillies, Kelsey Fry and Magill at Queen Mary’s Hospital in Sidcup. The surgical techniques for facial reconstruction that Gillies performed, including ‘the waltzing flap’, are well documented by the Tonks pastels collection, some of which are held at the Slade.
During the Second World War, another surgeon, Sir Archibald McIndoe, formed The Guinea Pig Club on whom he performed experimental reconstructive plastic surgery. Colin brought the lecture to life with a series of anecdotes including McIndoe unwittingly operating on Al Capone’s brother for which he received payment from a man carrying a violin case and an envelope containing $1,000.
Farming vs. Fabrication
The second portion of the lecture drew a comparison between the various methods used to get airborne during WW1 and the different possibilities when ‘growing tissues’, with the crux being that although modern tissue engineering seems like cutting edge research, the reality is like struggling with gravity using vintage planes.
Despite breakthroughs such as the first full face transplant in 2005, there is still a problem with the lifetime immunosuppression required, ruling out treatment for cancer.
The vacanti mouse, teeth grown on the kidneys of rabbits and Dolly the sheep: we had all heard of at least one case where tissue has been ‘cultivated’ using a method not unlike farming.
However, perhaps the most fascinating advances are taking place in the field of biomimetic engineering. We were given a lesson in making tissues from scratch following a pretty basic recipe.
Tissue is made from basic building blocks of proteins, cells and water which can be fabricated using 3D printing or collagen compression. Using techniques of layering and spiralling sheets of collagen filled with cells, adding spatial complexity such as groves and channels for blood vessels and nerves to grow, many types of tissue can be created: skin, bone, even corneas.
The question and answer session concluding the lecture elicited the complex realisation that despite the horrors of war, World War I and II created the environment of need that drove these advances in medicine.
Today, regulations prevent the kind of innovative surgery that McIndoe was practicing, and developments in artificial tissues that could be used to treat patients are restricted. Colin remonstrated that “there needs to be a change in our approach to innovative medicine in this country.” Lord Saatchi’s Medical Innovation Bill is one of the first steps to ensure that we are not stuck in the “dark ages” of reconstructive surgery.
Watch the full lecture below:
 Close
Close